Introduction
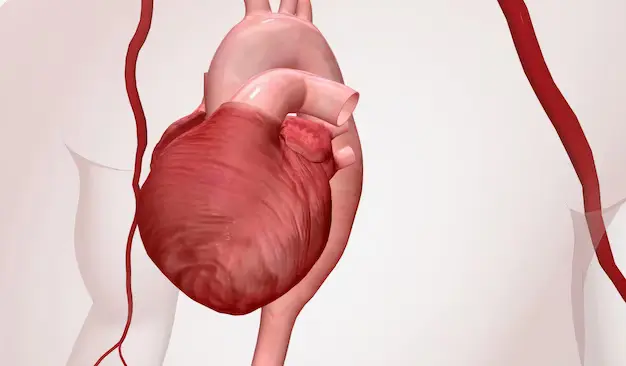
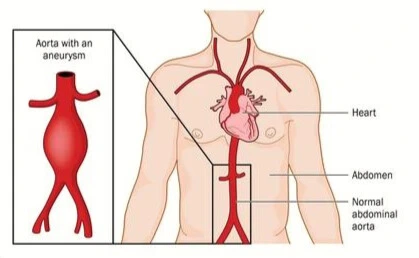
A thoracic aortic aneurysm (TAA) is a serious condition involving the aorta, the primary blood vessel originating from the heart and responsible for distributing blood throughout the body. Specifically affecting the upper portion of the aorta known as the thoracic aorta, this condition is characterized by the abnormal dilation or bulging of a segment of the vessel. Given the critical role of the aorta in systemic blood circulation, the presence of a thoracic aortic aneurysm poses a significant health risk. As the weakened area expands, there is an increased likelihood of complications such as dissection or rupture, which can lead to severe morbidity and mortality.
Anatomy
The anatomy of the thoracic aorta delineates a vital pathway for systemic blood circulation, originating just beyond the aortic valve and coursing through a distinctive trajectory. The ascending thoracic aorta, marked by its initial ascent and subsequent arch formation, plays a pivotal role by giving off coronary arteries and branching into the aortic arch vessels. While the typical configuration involves the brachiocephalic trunk, left carotid, and left subclavian arteries, variations in aortic arch anatomy are acknowledged.
Descending into the thoracic region, the aorta provides paired thoracic arteries, sequentially numbered from T1 to T12, and then descends adjacent to the spine. The journey continues through the hiatus of the diaphragm, transforming into the abdominal aorta. This abdominal segment extends retroperitoneally until its ultimate bifurcation into the common iliac arteries, a critical juncture occurring at the level of the fourth lumbar vertebra.
Pathophysiology
Aneurysm formation is a multifactorial process influenced by structural changes in the arterial wall, hemodynamic forces, and systemic conditions.
Aneurysms, characterized by a localized dilation of an arterial segment exceeding 50% of its normal diameter, primarily affect the infrarenal segment of the aorta. The size criteria for abdominal aortic aneurysms (AAAs) are defined by diameters greater than 3 cm, with the average infrarenal aorta size being 2 cm. Thoracic and thoracoabdominal aorta aneurysms are evaluated based on larger normal dimensions.
The medial layer of the aorta, crucial for tensile strength and elasticity, consists mainly of collagen and elastin. Variations in elastin content throughout the aorta may contribute to the increased frequency of aneurysms in specific regions.
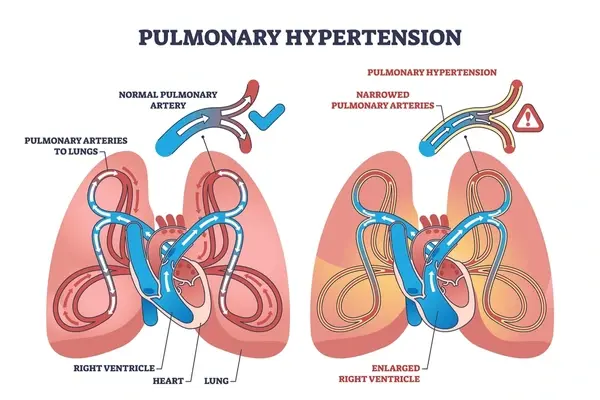
Enzymatic activity leading to the degradation of structural proteins, particularly elastin, weakens the aortic wall and promotes dilation. Hemodynamic factors, including low-resistance blood flow in the aorta and the impact of reflected arterial waves, play a role in aneurysm formation. Systemic hypertension further compounds the risk by accelerating aneurysm expansion.
The law of Laplace, describing the proportional relationship between wall tension, pressure, and the radius of the arterial conduit, emphasizes the critical role of increased wall tension in aneurysm progression. As aneurysm size and pressure rise, so does the risk of rupture.
Classification
Thoracic aortic aneurysms are classified based on their location within the aorta, extent of aortic involvement, and morphology.
-
General Anatomic Categories:
- Ascending Aortic Aneurysms (60%): From aortic valve to innominate artery.
- Aortic Arch Aneurysms (10%): Involving brachiocephalic vessels.
- Descending Aortic Aneurysms (40%): Distal to left subclavian artery.
- Thoracoabdominal Aneurysms (10%): Involving both thoracic and abdominal aorta.
-
-
Crawford-Safi Classification for Thoracoabdominal Aneurysms:
- Type I: Above the sixth intercostal space, involving celiac axis and superior mesenteric arteries.
- Type II: Extends distally to infrarenal aortic segment.
- Type III: Arises in distal half of descending thoracic aorta, extending into abdominal aorta.
- Type IV: Involves entire abdominal aorta from diaphragm to aortic bifurcation.
- Type V: Limited to visceral segment of abdominal aorta, arising in distal half of descending thoracic aorta.
-
- Fusiform: Uniform shape with symmetrical dilatation involving the entire aortic wall circumference.
- Saccular: More localized, appearing as an outpouching of only a portion of the aortic wall.
Etiology
Thoracic aortic aneurysms exhibit a diverse etiology, involving both degenerative and genetic factors, as well as various inflammatory and infectious conditions.
- Degenerative Factors and Atherosclerosis:
- Most TAAs are degenerative and associated with risk factors for atherosclerosis.
- The role of atherosclerosis in aneurysm formation remains unclear.
- Hypertension, smoking, and hypercholesterolemia are common risk factors.
- Connective Tissue Disorders: Syndromic TAAs are linked to connective tissue disorders such as Marfan, Loeys-Dietz, and Ehlers-Danlos syndromes. Nonsyndromic TAAs, without specific genetic syndromes, also have a significant familial component.
- Association with Other Aneurysms: Patients with TAAs may also have abdominal aortic aneurysms (AAAs). Coexistence of thoracic and cerebral aneurysms is possible, especially in patients with bicuspid aortic valves.
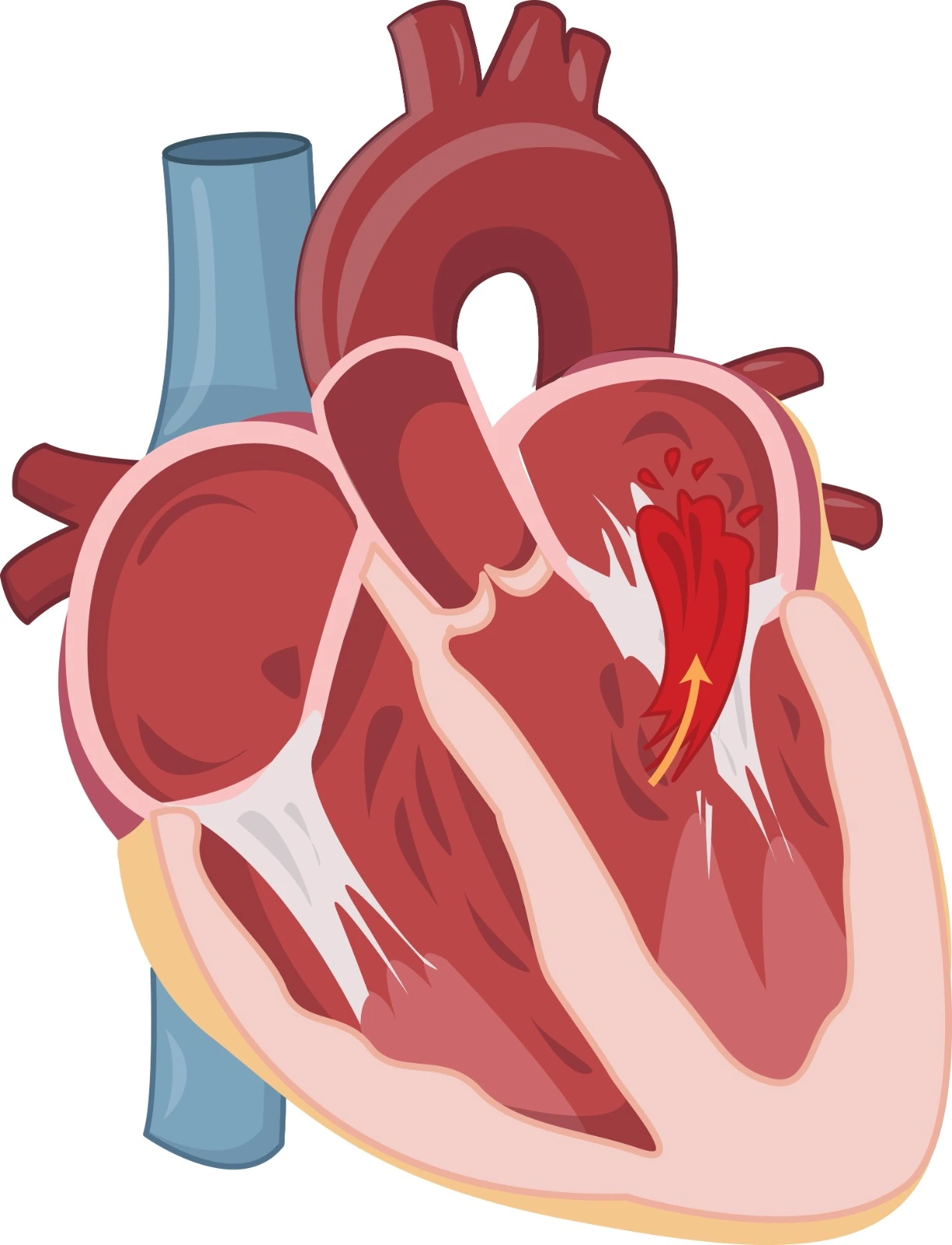
- Prior Aortic Dissection: Survivors of acute aortic dissection are at risk of progressive aortic expansion and late aortic rupture.
- Chest Trauma: may lead to pseudoaneurysms of the descending thoracic aorta.
- Aortitis: is a rare cause of TAA, linked to infectious or inflammatory conditions.
- Infectious Causes: particularly septic embolism, can lead to aneurysm formation in the thoracic aorta.
- Inflammatory Disorders: including giant cell arteritis and Takayasu arteritis, are associated with TAA development.
- Genetic Predisposition: Genetic defects affecting connective tissue metabolism contribute to about 5% of TAAs. Specific genetic syndromes like Marfan and Loeys-Dietz have distinct clinical features and aggressive aortic expansion.
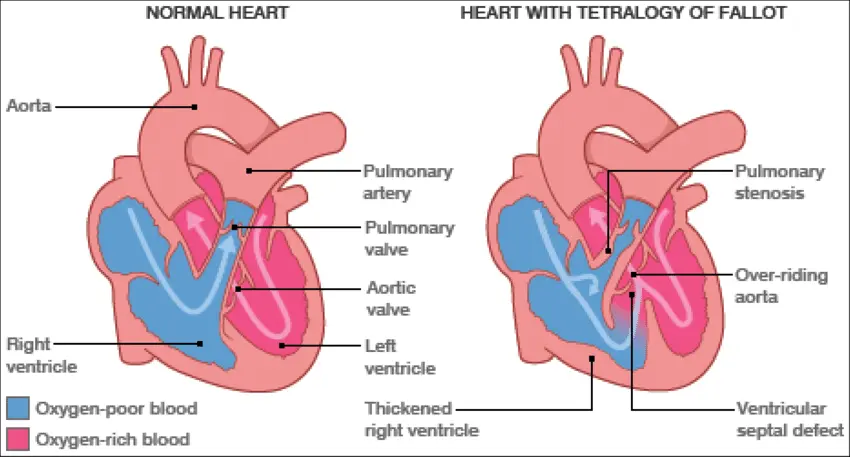
- Bicuspid Aortic Valve: Bicuspid aortic valve is associated with a higher risk of thoracic aortic aneurysms and aortic dissections.
- Aneurysm-Osteoarthritis Syndrome: A recently described syndrome, aneurysm-osteoarthritis syndrome, is caused by pathogenic variants in SMAD3, leading to aneurysms and arterial tortuosity.
Clinical Presentation
Asymptomatic Thoracic Aortic Aneurysm
Aortic aneurysms often remain asymptomatic until discovered incidentally through imaging studies or routine examinations.
Discovery Methods:
- Incidentally found on diagnostic tests such as echocardiography or CT scans.
- Screening for at-risk individuals may lead to the identification of aneurysms.
Screening Challenges:
- Biomarkers and gene expression profiles lack certainty in TAA identification.
- Genetic testing may reveal mutations associated with high-risk syndromes.
- Clinical markers, including physical features and associated conditions, aid in risk assessment.
Symptomatic Thoracic Aortic Aneurysm
- Presentation and Symptoms:
- Symptoms may arise due to rapid aneurysm expansion, increasing rupture risk.
- Surgical intervention is typically recommended once symptoms manifest.
- Symptoms include chest or abdominal pain, with variations based on aneurysm location.
-
- Complications and Severe Manifestations:
- Rupture is the most severe complication, presenting as severe chest pain and hypotension.
- Laboratory studies, including D-dimer, guide management and assess severity.
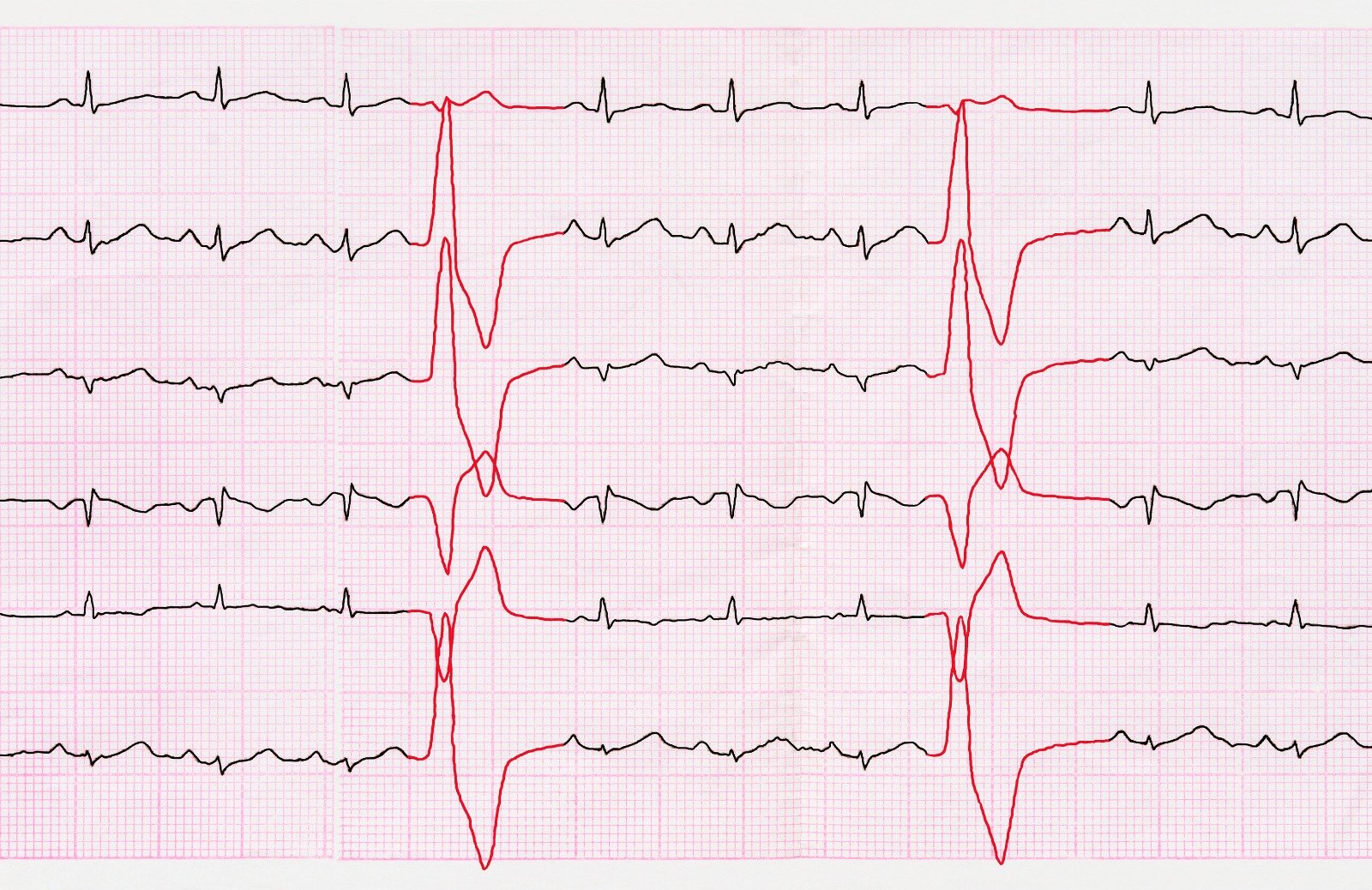
- Electrocardiography may reveal myocardial infarction signs in ascending aortic aneurysms.
-
- Initial laboratory tests include CBC, electrolytes, D-dimer, and markers of cardiac ischemia.
- ECG is performed for chest pain symptoms, revealing myocardial infarction or hypertrophy.
- Anemia and elevated lactic acid levels provide additional diagnostic insights.
Diagnosis
Physical examination
The physical examination plays a crucial role in the assessment of patients with suspected thoracic aortic aneurysm (TAA), especially those with risk factors or acute symptoms. Key components of the examination include vital signs, thorough cardiovascular assessment, evaluation of upper extremity blood pressures, and identification of specific physical characteristics associated with high-risk conditions.
Vital signs, including sinus tachycardia or hypotension, may provide important clues, and the presence of fever could indicate an infected aneurysm. In cases of ruptured TAA, assessing femoral and pedal pulses is essential, and the use of a handheld continuous wave Doppler may aid in identifying lower extremity pulses. The examination should also focus on physical features related to high-risk conditions:
- Marfan Syndrome: Characteristics such as tall stature, scoliosis, pectus deformities, elongated skeletal features, hyperflexibility, and ocular abnormalities, including ectopia lentis, may be present.
- Loeys-Dietz Syndrome: Overlapping features with Marfan syndrome, but specific characteristics such as bifid uvula, hypertelorism, and cervical arterial tortuosity are more commonly associated with Loeys-Dietz syndrome.
- Familial TAA: Associated features may include livedo reticularis, iris flocculi, congenital mydriasis (ACTA2 mutation), and peripheral vascular malformations.
Laboratory Studies
Several laboratory studies are crucial for a comprehensive assessment and management of patients with suspected thoracic aortic aneurysm or acute complications. The recommended laboratory studies include:
- Complete Blood Count (CBC): Provides information on red and white blood cell counts, helping to assess for anemia, infection, or other hematological abnormalities.
- Electrolyte Evaluation and Blood Urea Nitrogen (BUN)/Creatinine: Essential for evaluating renal function, which is critical for stratifying morbidity, especially in the context of potential surgical interventions.
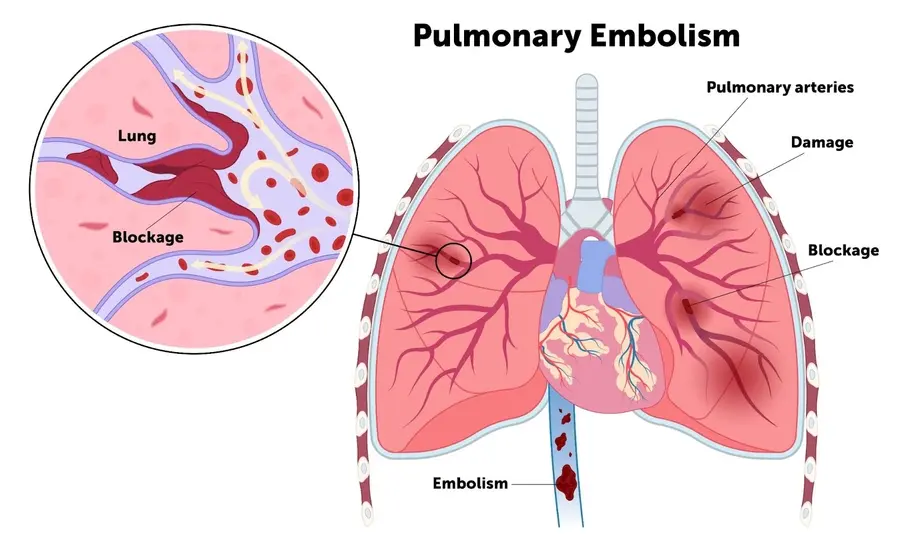
- Prothrombin Time (PT), International Normalized Ratio (INR), and Activated Partial Thromboplastin Time (aPTT): Assess coagulation status and help guide anticoagulation strategies, particularly important in patients at risk for thromboembolic events.
- Blood Type and Crossmatch: Essential for immediate availability of compatible blood products in case of surgical intervention or significant bleeding.
- Liver Function Tests (LFTs) and Amylase/Lactate Values: Indicated for patients with acute dissection or those at risk of distal embolization. LFTs can assess liver function, while amylase and lactate values aid in evaluating potential complications such as visceral ischemia.
Imaging Studies
In the diagnostic evaluation of thoracic aortic aneurysms (TAAs), various imaging studies play a crucial role in providing detailed anatomical information. Here are the key imaging modalities and their respective contributions:
- Chest Radiography.
- Echocardiography.
- Ultrasonography.
- Intraoperative Imaging: Intraoperative intravascular ultrasonography (IVUS) & Epiaortic ultrasonography.
- Aortography.
- Computed Tomography (CT).
- Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA).
Other Tests
In the preoperative evaluation of patients with thoracic aortic aneurysms (TAAs), a comprehensive assessment is essential to ensure optimal management and minimize perioperative risks. Here are the recommended evaluations based on specific patient characteristics:
- Baseline Electrocardiography (ECG).
- Transthoracic Echocardiography (TTE).
- Pulmonary Function Tests with Spirometry.
- Room-Air Arterial Blood Gas Determinations.
- Cardiac Catheterization.
Treatment & Management
Lifestyle Modification and Smoking Cessation:
- Thoracic AA patients advised to quit smoking and referred to cessation programs.
- Active smoking is identified as a major risk factor for developing thoracic AA.
Dyslipidemia Management:
- Atorvastatin or rosuvastatin recommended for individuals with thoracic AA.
- Statin therapy is associated with a significant reduction in all-cause mortality and composite endpoints.
Blood Pressure Control:
- Hypertension control is crucial to reduce myocardial infarction, stroke, heart failure, death, and aortic dissection.
- Target blood pressure for thoracic AA patients: <130/80 mmHg.
- Combined beta-blocker and ACE inhibitor or ARB therapy recommended.
Surgical Intervention Criteria:
- Asymptomatic surgical candidates: Ascending thoracic aorta or aortic sinus diameter ≥5.5 cm.
- Genetic conditions (e.g., Marfan's syndrome): Elective surgery for diameters between 4.0 and 5.0 cm.
- Marfan's syndrome women desiring pregnancy: Surgery if ascending thoracic aorta diameter >4.0 cm.
- Bicuspid aortic valve patients: Surgery if ascending thoracic aorta diameter >5.5 cm or >5.0 cm with family history or increased diameter ≥0.5 cm/year.
Aortic Dissection Management:
- Decrease aortic shear stress with beta-blockers as the initial choice.
- Target systolic blood pressure: 100-120 mmHg; ventricular rate <60 beats/minute.
- Additional drugs (e.g., verapamil, diltiazem, sodium nitroprusside) if needed for blood pressure control.
- Medical treatment may be sufficient for some type B dissections, with beta-blockers improving survival.
Long-Term Follow-up and Survival:
- Statin therapy is associated with improved long-term survival and reduced surgery rates.
- Beta-blockers improve survival in acute aortic dissection, and calcium channel blockers are beneficial for type B dissection.
References:
- Tseng, E. (n.d.). Thoracic Aortic Aneurysm Treatment & Management: Approach Considerations, Medical Therapy, Surgical Options. https://emedicine.medscape.com/article/424904-treatment#showall
- Clinical manifestations and diagnosis of thoracic aortic aneurysm. (n.d.). UpToDate. Retrieved December 26, 2023, from https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-thoracic-aortic-aneurysm
- Epidemiology, risk factors, pathogenesis, and natural history of thoracic aortic aneurysm and dissection. (n.d.). UpToDate. Retrieved December 26, 2023, from https://www.uptodate.com/contents/epidemiology-risk-factors-pathogenesis-and-natural-history-of-thoracic-aortic-aneurysm-and-dissection
- Faiza, Z. (2023, May 1). Thoracic Aorta Aneurysm. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK554567/
- Aronow, W. S. (2018, February 1). Treatment of thoracic aortic aneurysm. Annals of Translational Medicine. https://doi.org/10.21037/atm.2018.01.07


.webp)
.webp)
.webp)
.webp)
.webp)

.webp)