Unstable Angina is a manifestation of Acute Coronary Syndrome (ACS). It is resulted from a significant impedance of the blood flow in one of the coronary arteries that nourished the myocardium. It is considered a medical emergency situation that requires transfer to the hospital for urgent management, as it may aggravate to a Heart Attack, and is associated with a high risk of death.
Pathophysiology
Elevated myocardial oxygen demand due to:
- Fever.
- Hyper-metabolic status.
- Obstructive cardiomyopathy.
- Cardiac failure.
- Aortic stenosis.
- Arrhythmia, or irregular heartbeat,.
- High output status.
- Improper coronary artery oxygen supply due to anemia.
- Hypertension
Can contribute to myocardial ischemia.
Atherosclerosis is considered the main underlying cause of unstable angina. As Atherosclerosis induces the formation of outgrowing plaque of the lipid core covered by the fibromuscular cap, that leads to narrowing in coronary arteries and subsequent myocardial ischemia. Intraplaque proteases and elastases, along with shearing forces from blood flow and endothelial wall stress, can cause moderate to large disturbances in atherosclerotic plaque that may lead to its rupture.
Exposure to collagen and other subendothelial components will activate platelet adhesion and aggregation. Platelets will release cytokines that induce vasoconstriction and lead to the activation of the coagulation cascade and the formation of a thrombus, which is further stabilized by fibrin activation. As a result, a significant coronary artery stenosis will occur, which will be sufficient to induce clinical symptoms.
Although the thrombus in unstable angina is considered to be a non-occlusive thrombus, that is not associated with myocardial infarction and cardiac biomarkers release from necrotic myocardial tissue into blood circulation, it is associated with a high risk of developing into an occlusive thrombus.
Genetic factor
Studies have identified some genes that may be linked with unstable angina, as in chromosome 2q36-q37.3, chromosome 3q26-q27, and chromosome 20q11-13. In addition, a polymorphism in glycoprotein Ia may affect platelet aggregation timing, a polymorphism in the matrix metalloproteinase (MMP) gene is linked with poor prognosis, and some polymorphisms in interleukin-related genes are suspected to be linked with the development of unstable angina.
Clinical Presentation
Patients with unstable angina are typically present with sudden retrosternal chest pain that can be radiate to the shoulders, arms, neck, or jaw. Other symptoms, such as palpitations, dyspnea, diaphoresis, dizziness, nausea and vomiting can also present. Unstable angina chest pain is known to be with persistent intensity that may get worse over time, and it is not only induced by excretion, nor completely alleviated with rest or Nitroglycerine. Lasts longer than 15 to 20 minutes.
Unstable angina may lead to hemodynamic instability and microembolism formation, which are accompanied by Stroke, Myocardial Infarction, Heart Failure, Arrhythmias, and Valvular Disease.
Prognosis Estimation
Thrombolysis in Myocardial Infarction (TIMI) Risk Score is used as a prognostic tool, based on a scale out of 7points.

Classification
Braunwald Classification of Unstable Angina:

Diagnosis
Initial assessment and urgent testing must be done for the diagnosis of unstable angina and the selection of appropriate management.
- Obtaining a full patient history is essential for identifying the probable coronary disease.
- Physical examination is usually unremarkable in case of unstable angina, as it is not sensitive and specific. But, it may play a role in ruling out other conditions.
- Laboratory tests have a role in myocardial infarction diagnosis, and general assessment of the patient
- Serial testing of cardiac biomarkers, including high sensitivity cardiac troponins I and T. It is performed to determine if any of the myocardium has infarcted.
- Pro-brain natriuretic peptide level is associated with mortality risk, and is used for Heart Failure screening, diagnosis, and prognosis assessment.
- Lipid profile.
- Coagulation profile.
- Kidney function test.
- Electrolytes level.
- Complete blood count for anemia screening as a participating factor.
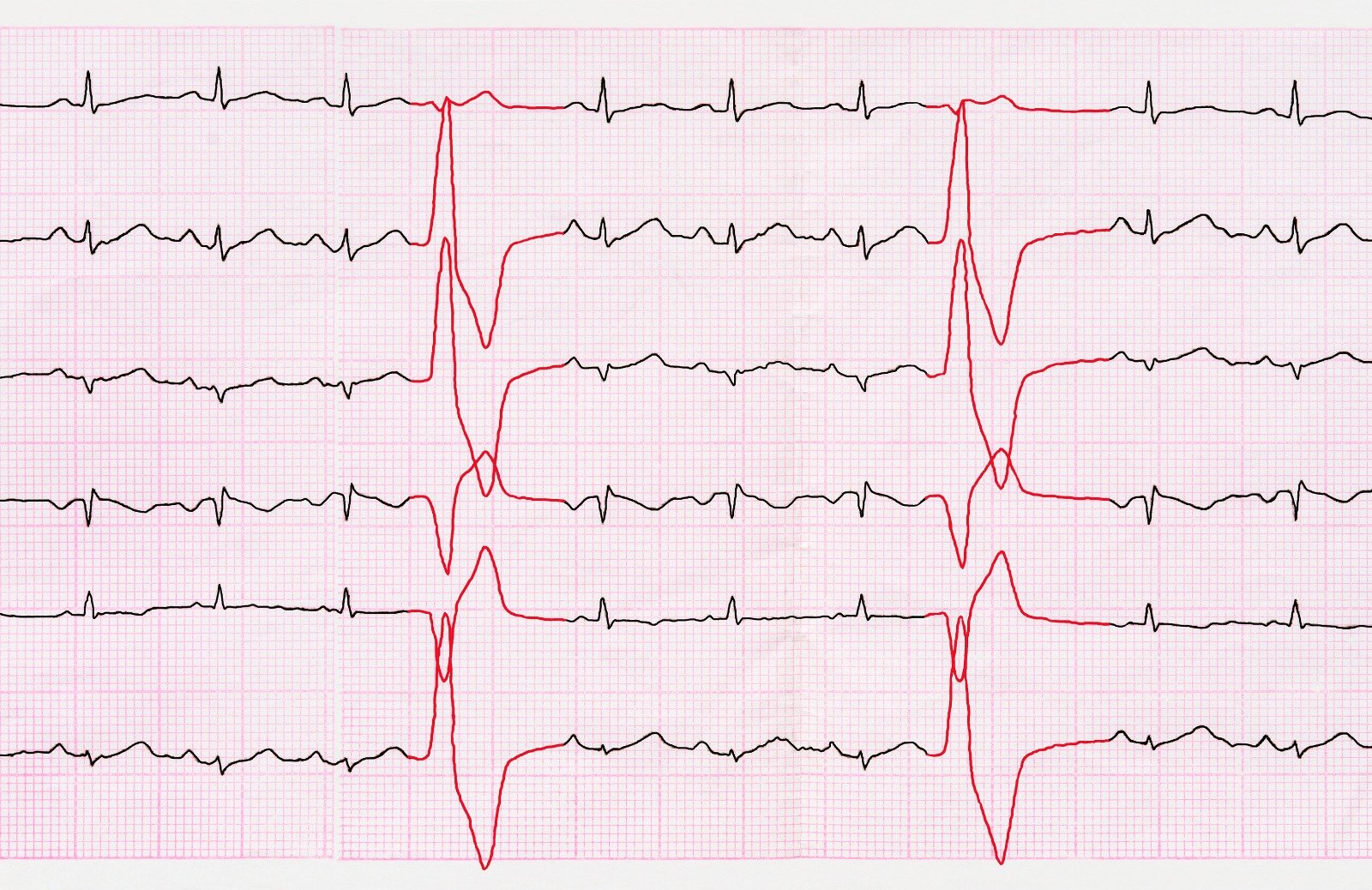
- Serial Electrocardiography is used to exclude electrical changes associated with myocardial infarction, and to detect any arrhythmia.
- Echocardiography is used for left ventricular dysfunction diagnosis or prognosis evaluation.
- Chest X-ray is used to assess heart size, dissection, and other pulmonary conditions.
- Magnetic resonance imaging (MRI) can be used to detect myocardial ischemia, infarction, or scarring.
- Exercise testing may be done as part of the predischarge assessment.
References
https://www.heart.org/en/health-topics/heart-attack/angina-chest-pain/unstable-angina
https://www.ncbi.nlm.nih.gov/books/NBK442000/
https://emedicine.medscape.com/article/159383-overview#a1


.webp)
.webp)


.webp)



.webp)

.webp)



.webp)