Overview
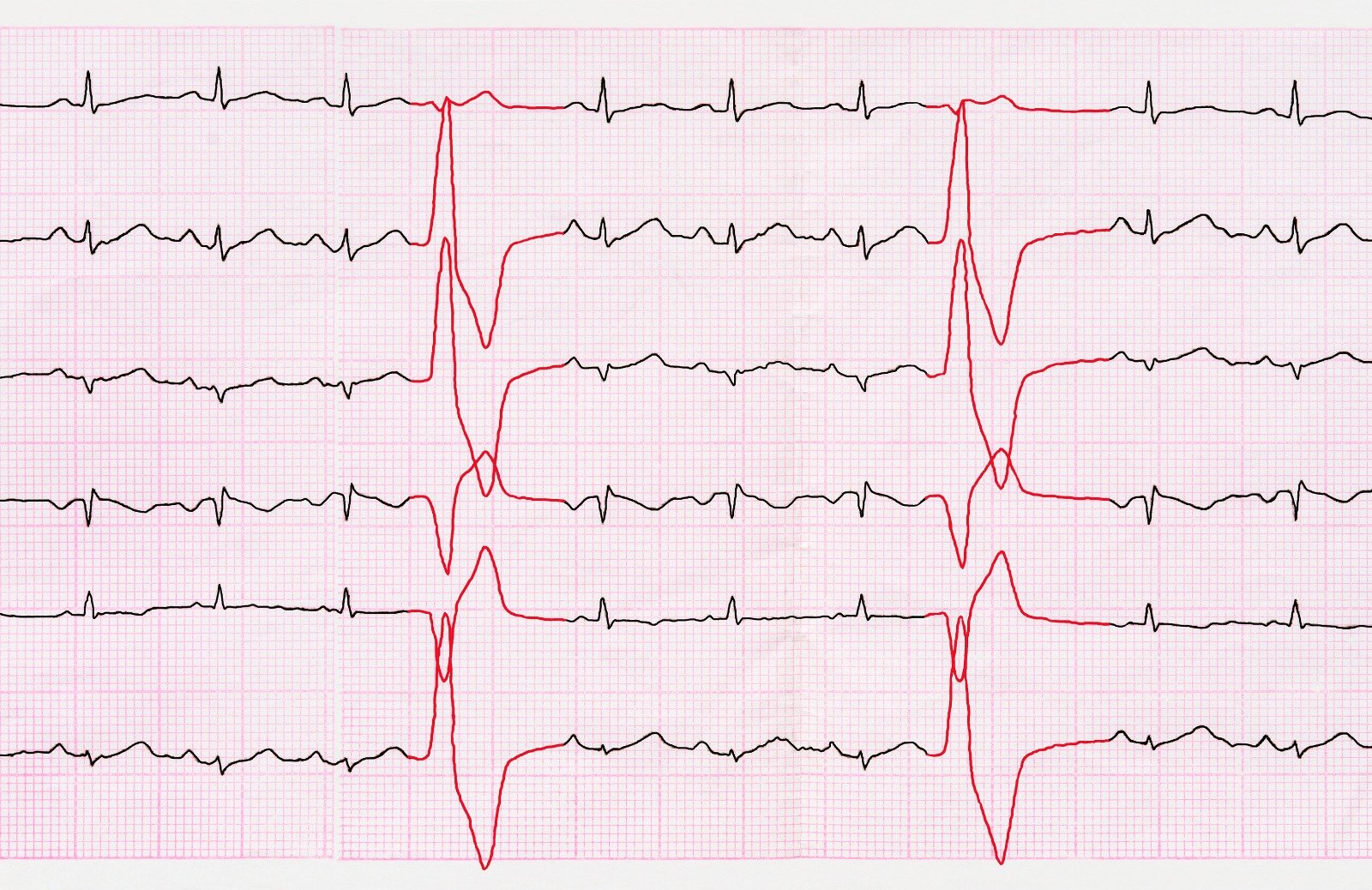
Wolff-Parkinson’s white syndrome is considered a congenital abnormality that is associated with abnormal conductivity between the atria and the ventricles, creating a preexcitation syndrome. It is characterized by the presence of an electrical “accessory pathway” that connects the atria and ventricles and bypasses the AV node. Symptoms vary from mild palpitations to syncope, presyncope, or even cardiac arrest and sudden cardiac death.
Treatment of acute symptomatic Arrhythmia
The treatment of choice for symptomatic patients is catheter-based radiofrequency ablation. This is due to its high success rate and low-risk profile, but cryoablation can also be utilized.
Some patients might require initial pharmacological therapy for rate control or for restoring normal sinus rhythm. This approach to rate control should be done cautiously since there are electrophysiological changes between AV nodal tissue and accessory pathway tissue, and when used for patients with tachycardia involving accessory pathways, it might lead to a worsening of symptoms.
An initial assessment should be done for all patients with tachycardia, especially if the involvement of an accessory pathway is suspected. Treatment is initiated based on the patient's hemodynamic stability, and the approach is done as follows; evaluation and treatment based on arrhythmia type in stable patients, whereas hemodynamically unstable patients who present with hypotension, altered mental status, shock signs, ischemic chest discomfort, or acute heart failure should undergo urgent electrical cardioversion or defibrillation.
Orthodromic atrioventricular reciprocating tachycardia (AVRT)
A step-wise approach is usually applied. Vagal maneuvers (Valsalva maneuver, carotid sinus massage) are the initial interventions and are capable of causing AV node block and terminating tachycardia in many patients.
If medications were not effective, pharmacological therapy should be initiated:
- Adenosine is the first line option.
- If adenosine wasn't effective, then verapamil is the second-line option.
- Procainamide or beta-blockers (propranolol, metoprolol, and esmolol) are the next steps if adenosine and verapamil are not effective. Procainamide is preferred when there is QRS complex tachycardia due to chronic bundle branch block or when the diagnosis of orthodromic AVRT isn't certain.
For permanent junctional reciprocating tachycardia (PJRT) caused by slowly conducting accessory pathways, ablation of the accessory pathway is the preferred approach. However, if the patient presents with an acute symptomatic PJRT, treatment can be initiated similarly to that of conventional orthodromic AVRT:
- Adenosine Verapamil: can interrupt PJRT for a few beats.
- IV Procainamide: provides longer-lasting interruption.
- Oral Flecainide: an effective approach for controlling the situation before ablation
Antidromic AVTR
If suspected AVTR is strictly regular and monomorphic: adenosine can be tried. Treatment failure can suggest a second accessory pathway; in such cases, procainamide or amiodarone should be considered.
For most suspected or known AVTR: procainamide is the agent of choice.
For undiagnosed wide complex tachycardia: in patients with uncertain diagnosis and etiology, ventricular tachycardia should be assumed, and patients can be treated accordingly.
AFIB with preexitation
- Therapy goals are: to control ventricular response and terminate AFIB.
- Adenosine, Verapamil, Beta-blockers, Amiodarone, Digoxin, and Diltiazem should be avoided.
- Hemodynamically unstable patients: urgent electrical cardioversion.
- Hemodynamically stable patients: Procainamide or Ibutilide
- Flecainide and propafenone can be used, but the paranormal form isn't available in some countries.
Prevention of recurrent Arrhythmia
1. Catheter ablation is preferred over pharmacological therapy in symptomatic patients with accessory pathways who have orthodromic AVRT, antidromic AVRT, and are excited AF or atrial flutter, whereas surgical ablation is less preferred unless the patient is highly symptomatic, hemodynamically unstable, has a drug-refractory arrhythmia, and radiofrequency ablation has failed.
Indications of ablation:
- symptomatic tachyarrhythmia.
- Careers that put a risk on the patient if they develop symptoms (truck drivers, athletes, etc.)
- Selected asymptomatic patients
2. Medical therapy
- Recurrent Orthodromic AVRT:
- Flecainide and propafenone are the first options.
- Beta-blockers might be occasionally used as a second-line option in patients with low-risk WPW accessory pathways.
- Amiodarone might be used, but it has multiple adverse events that make it unfavorable.
- Recurrent antidromic AVRT:
- Ablation is the preferred approach.
- In patients who refuse ablation or who are not candidates for ablation, pharmacological therapy can be initiated. Flecainide and propafenone are the agents of choice.
- Amiodarone can be used, but it is not preferred because of its adverse effects.
- Recurrent pre-excited AFIB:
- Ablation is the preferred approach.
- In patients who refuse ablation or who are not candidates for ablation, flecainide and propafenone are the best choices.
- Amiodarone can be used when classes IC and IA are ineffective, when ablation isn't appropriate, or when ablation has failed.
- Never use amiodarone in the acute management of AFIB.
References
- https://www.ncbi.nlm.nih.gov/books/NBK554437/
- https://www.uptodate.com/contents/treatment-of-arrhythmias-associated-with-the-wolff-parkinson-white-syndrome


.webp)
.webp)
.webp)


.webp)



.webp)

.webp)