Pulmonary hypertension is a condition in which blood pressure increases within the lung arteries. In this condition, the blood vessels that carry blood from the heart to the lungs become narrow and blocked, this makes the heart work harder than normal to pump blood into the lungs.
Anatomy
The main pulmonary artery ,known as the pulmonary trunk, is located along the left side of aorta, and is about 5 cm in length and 3 cm in diameter. Pulmonary artery wall consists of 3 main layers:
- The tunica adventitia, the outermost layer, is the strongest of the three layers.
- Tunica media, a middle layer that pushes blood through.
- Tunica intima, a smooth inner layer.
Underneath aortic arch, it is further divided into right and left pulmonary arteries that are located on the anterior side of mainstem bronchus and directed toward right and left lung, respectively.
Physiology
In Pulmonary circulation, unoxygenated blood normally flows at low pressure from the right ventricle through pulmonary valve into pulmonary artery, and then to the lungs. After that, gas exchange occurs, and oxygenated blood goes back to the left atrium through pulmonary vein. Hypertrophy of pulmonary artery wall and lumen narrowing will lead to elevation in pulmonary artery pressure which will affect blood flow and oxygenation process.
Etiology
World Health Organization (WHO) has divided Pulmonary Hypertension into five groups based on the underlying cause:
- Group 1: Pulmonary arterial Hypertension (PAH). Where pulmonary vascular resistance is elevated due to hyperthrombotic status, or endothelium dysfunction which lead to vasoconstriction, or vascular remodeling and arterial wall hypertrophy.
- Group 2: Pulmonary Hypertension induced by left-sided Heart Failure.
- Group 3: Pulmonary Hypertension due to lung disease with or without hypoxia.
- Group 4: Chronic Thromboembolic Pulmonary Hypertension (CTEPH), which is caused by blood clots in the lungs or general clotting disorders.
- Group 5: Pulmonary Hypertension with unclear or multifactorial etiologies .It includes hematologic disorders such as myeloproliferative disorders, systemic disorders such as Sarcoidosis and Vasculitis, metabolic disorders such as Thyroid dysfunction, and miscellaneous conditions such as tumor obstruction, and dialysis.
Diagnostics
Multiple tests and exams may be performed to diagnose Pulmonary Hypertension, and identify the underlying cause and complications:
- Physical examination may identify peripheral edema, ascites, or hepatomegaly if correlated right sided Heart Failure has developed.
- Heart auscultation may reveal a boost in intensity of pulmonary component of second heart sound (P2), and a split in P2. In addition, fourth heart sound (S4) on right side and parasternal heave on left side may be noticed. Moreover, high-pitched systolic murmur with tricuspid valve regurgitation and third heart sound (S3) may be heard in patients with associated right-sided Heart Failure.
- Routine laboratory tests can be performed to assess the underlying cause.
- Chest X-ray, cardiac Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) can be used to detect lung disorders and any change in heart size.
- Pulmonary function test and sleep study can be used to identify the underlying cause.
- Echocardiogram is used to diagnose Pulmonary Hypertension and assess management efficacy.
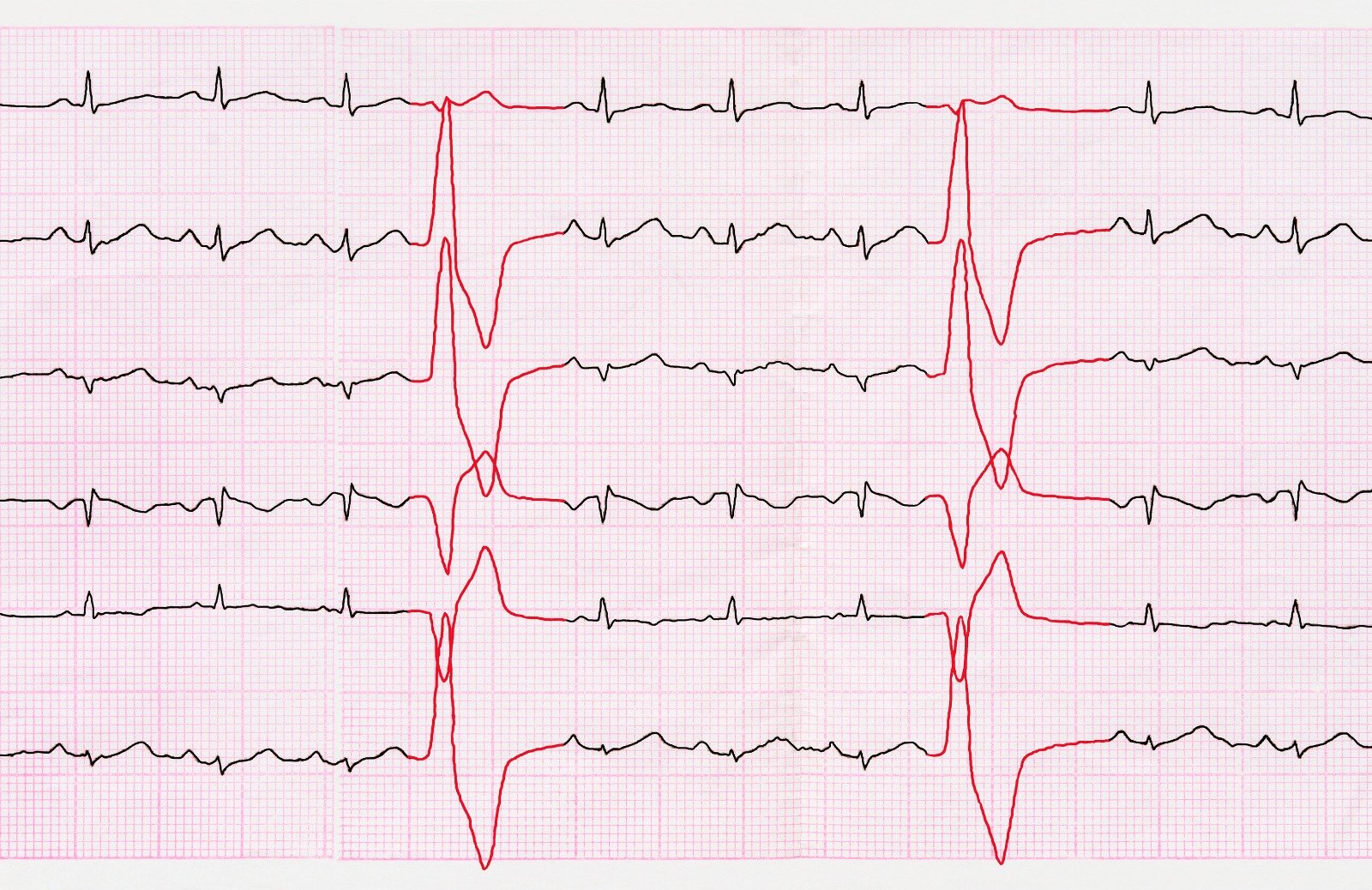
- Electrical cardiogram (ECG) can detect electrical heart abnormalities and arrhythmias.
- Assessment of jugular vein waves may detect a prominent A wave.
Pulmonary Hypertension diagnosis is confirmed when pulmonary artery pressure is elevated above 25 mmHg at rest, or above 30 mmHg during physical activity, which is measured through right heart catheterization.
Clinical presentation
Patients with Pulmonary Hypertension may be asymptomatic for a longtime, while others may present with frequent symptoms, which become more significant with disease progression, as they include:
- Shortness of breath.
- Cough.
- Chest pain.
- Upper right side abdominal pain.
- Tachycardia.
- Light headache.
- Fatigue
- Poor appetite.
- Pale skin and peripheral edema.
Classification
Patients with confirmed Pulmonary Hypertension are classified into several classes based on symptoms:
- Class I: Asymptomatic patients.
- Class II: Patients with symptoms induced by physical activity, which cause slight limitation of daily activities.
- Class III: Patients complain from symptoms triggered by any simple activity, which cause significant limitation of physical activities.
- Class IV: Patients with symptoms noticed even at rest.
Progression and Complications
Pulmonary Hypertension progression and mortality risk are dependent on condition severity, underlying cause and management.
- Pulmonary Hypertension is associated with progressive pulmonary vascular resistance. As a result, the right ventricle of heart tries to compensate by increasing the pumping force to overcome the resistance. Over time, compensation will fail, which may lead to right sided Heart Failure, and an increased risk of Arrhythmias and sudden cardiac death.
- Pulmonary Hypertension may result in pulmonary artery dilation, dissection or rupture, and it may compress the left main coronary artery.
- Hypoxia and vasoconstriction of pulmonary artery may lead to the development of collateral bronchial arteries which is associated with hemoptysis risk.
References
- https://www.ncbi.nlm.nih.gov/books/NBK534812/
- https://my.clevelandclinic.org/health/body/21486-pulmonary-arteries
- https://www.cdc.gov/heartdisease/pulmonary_hypertension.htm
- https://emedicine.medscape.com/article/303098-overview
- https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure/pulmonary-hypertension-high-blood-pressure-in-the-heart-to-lung-system
- https://www.mayoclinic.org/diseases-conditions/pulmonary-hypertension/diagnosis-treatment/drc-20350702



.webp)
.webp)

.webp)



.webp)

.webp)



.webp)