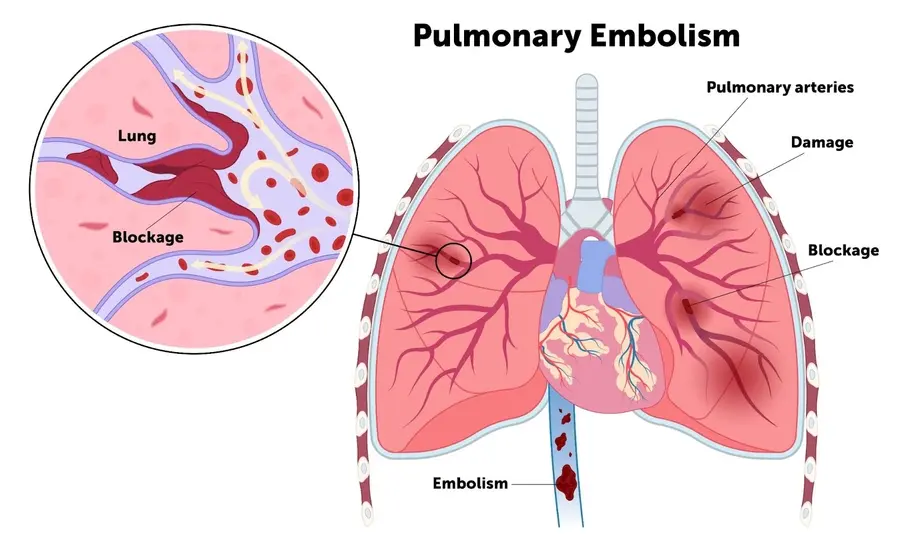
Deep vein thrombosis is a form of venous thromboembolism (VTE). It is related to thrombus formation in a venous conduit of a deep muscle, more often at extremities. It may resolve spontaneously as the body can dissolve it directly without any complications, while it may be associated with an elevated risk of emboli formation that may move and reach the lungs, causing a serious life threatening pulmonary embolism (PE).
Anatomy
Peripheral venous circulation consists of suprafascial collecting veins, which have a thin distensible wall to work as blood reservoirs, and secondary subfascial conduit veins, such as anterior tibial veins, posterior tibial veins, peroneal veins, popliteal vein, femoral vein, deep femoral vein, common femoral vein and iliac vein, that have a thick and tight wall and allow venous blood to return back to the heart when working together with deep calf muscles.
Pathophysiology
Blood circulation disturbances that cause blood stasis, blood clotting abnormalities linked to increased thrombosis tendency, and blood vessel wall damage that activates the coagulation cascade all combine to form the Virchow triad that elucidates vascular thrombosis contributing factors. In addition, deep vein thrombosis of the upper extremities can occur due to chronic venous compression by musculoskeletal structure, as in the case of Paget-von Schrötter syndrome.
Risk factors
- Previous or family history of deep vein thrombosis.
- Inherited or acquired disorders of coagulation/fibrinolysis.
- Advance age.
- Immobility or decreased mobility, as in prolonged sitting or hospitalization, and hip or knee replacement surgeries.
- Trauma induced by major surgeries or central venous catheter replacement.
- Acute infections.
- Chronic Inflammatory disorders.
- Varicose veins.
- Burns.
- Malignancy.
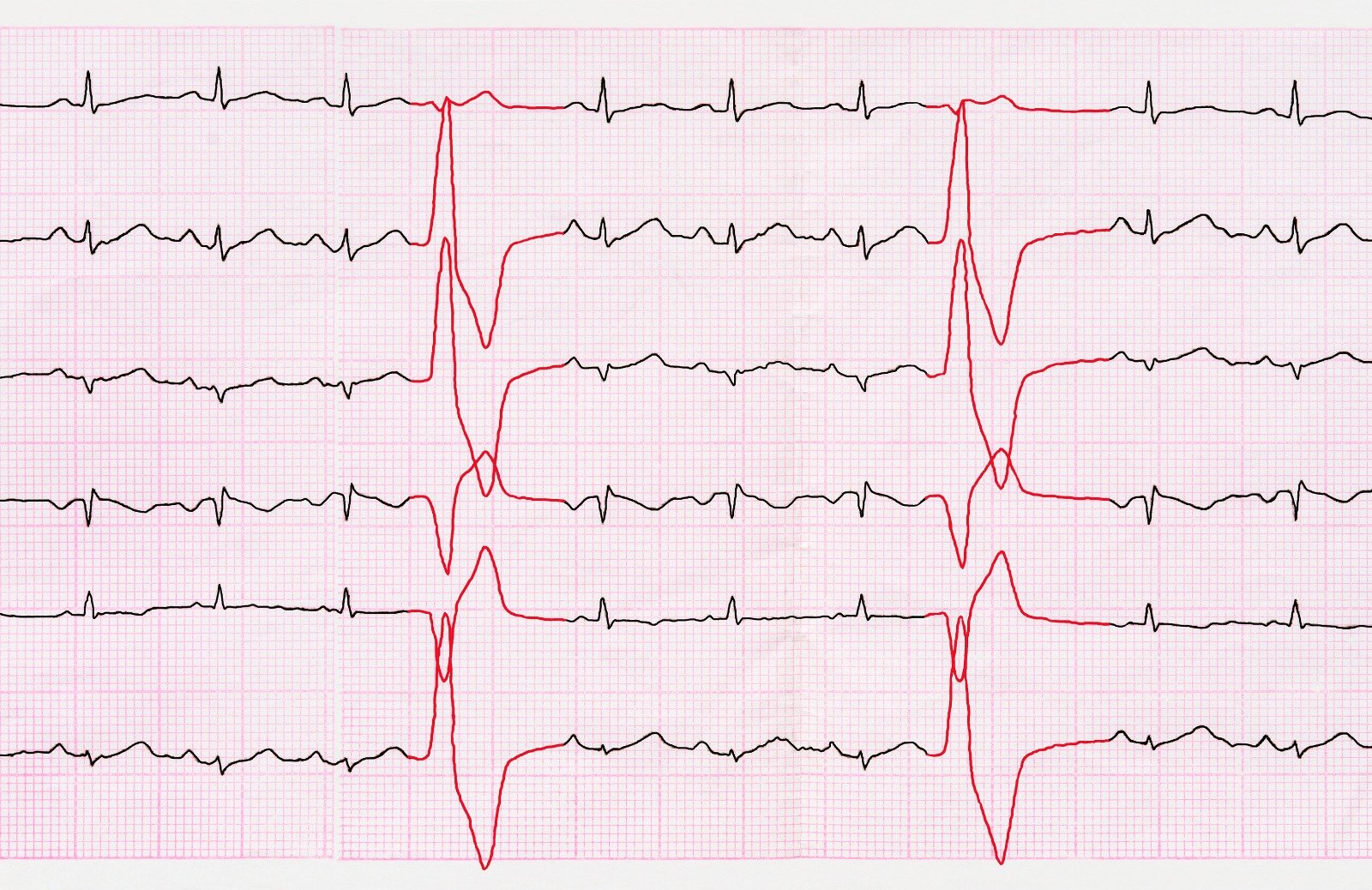
- Stroke or Myocardial Infarction.
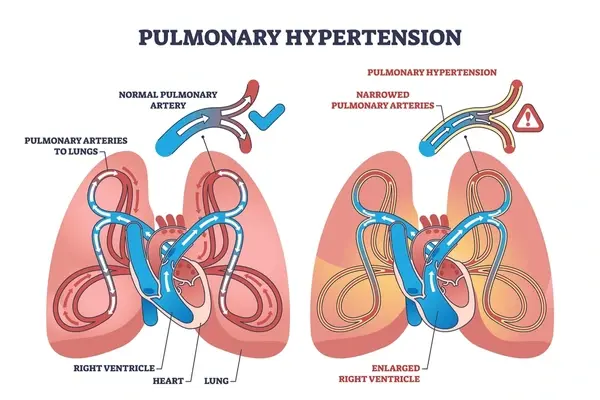
- Heart Failure.
- Pregnancy and postpartum.
- Usage of Contraceptives or hormonal replacement therapy.
- Obesity.
- Smoking.
Clinical Presentation
- Patients with deep vein thrombosis may be asymptomatic or present with throbbing pain, swelling and tenderness in the affected area, as well as redness or darkness or a warm sensation in the surrounding skin.
- The Patient may present with shortness of breath, chest pain, cough, tachycardia and dizziness if deep vein thrombosis is complicated by pulmonary embolism.
- Delayed symptoms of extremity heaviness, pain, skin discoloration, rash and itchiness can be noticed if the patient develops post-thrombotic syndrome where venous wall or valve is damaged.
Lower extremity Deep vein Thrombosis Types
- Distal DVT: it is limited to veins below the knee. It is associated with lower risk of complications and recurrence.
- Proximal DVT: it involves popliteal vein or other proximal vein (Above the knee). It is considered the most common type.
- Iliofemoral DVT: it involves thrombosis in iliac or femoral vein. It is associated with higher risk of complications and recurrence.
Diagnosis
- Routine laboratory tests: can identify patients at risk, such as antithrombin III level, N-terminal pro-brain natriuretic peptide (NT-proBNP), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR).
- Physical examination: can be useful to strengthen the probability of deep vain thrombosis diagnosis, but alone is not sufficient to confirm the diagnosis.
- Homans sign; a discomfort in the calf muscles when foot is in forced dorsiflexion while knee is in straight position.
- Phlegmasia alba dolens, a clinical triad of pain, edema and discoloration of involved extremity which described as phlegmasia cerulea dolens. It is also known as milk leg syndrome when associated with iliac vein compression.
- Palpable and stuffed venous segment.
- American Academy of Family Physicians (AAFP)/American College of Physicians (ACP): recommendations regarding workup if DVT is suspected:
- Use Well's criteria to assess DVT risk in out-sitting patients and patients presented to emergency department. While using the Oudega rule to assess the risk for patients in primary care settings.
- High sensitivity D-dimer test is recommended in patients with low DVT probability. As a negative result is used to role out DVT, while a positive result require a duplex ultrasonography to confirm the diagnosis.
- Ultrasonography is the first line imaging examination to confirm diagnosis in patients with high DVT probability. Other available imaging exams include venography, impedance plethysmography, magnetic resonance imaging (MRI), and nuclear imaging.
- Ventilation-perfusion (V/Q) scan, multidetector helical computed axial tomography (CT), and pulmonary angiography can be used in patients with intermediate-high risk of pulmonary embolism.

References
https://www.ncbi.nlm.nih.gov/books/NBK425364/
https://www.nhs.uk/conditions/deep-vein-thrombosis-dvt/
https://www.dynamed.com/condition/deep-vein-thrombosis-dvt
https://emedicine.medscape.com/article/1911303-overview#a1


.webp)
.webp)
.webp)
.webp)
.webp)

.webp)