Introduction
Pericardial effusion denotes the atypical accumulation of fluid in the pericardial sac enveloping the heart. This sac is composed of two layers: the delicate visceral pericardium, formed by a single layer of cells tightly affixed to the heart's epicardium, and the sturdier, fibrous parietal pericardium, composed of collagen and elastin. The parietal pericardium adheres to various structures, including the lungs, diaphragm, sternum, great vessels, and other mediastinal structures encircling the heart.
Pathophysiology
The clinical implications of pericardial effusion hinge on the rate at which fluid accumulates within the pericardial sac. Swift accumulation, even as little as 80 mL, can elevate intrapericardial pressures, while gradual buildup may reach 2 L without symptoms. Understanding the pericardium's properties is crucial for anticipating cardiac changes during physiologic stress.
The pericardium significantly contributes to ventricular interdependence, distributing forces across the heart and linking the function of one ventricle to another. During inspiration, it restrains left-sided chamber dilation, influencing cardiac output. However, in the presence of rising intrapericardial pressures, as seen in pericardial effusion, this effect intensifies, potentially leading to a notable reduction in stroke volume and progressing to pericardial tamponade.
Additionally, the pericardium serves a protective role during hypervolemic states by limiting acute cardiac cavitary dilatation. Recognizing these dynamic interactions between the pericardium and cardiac function is essential for a comprehensive understanding of pericardial effusion and its potential impact on cardiovascular health.
Etiology
The causes of pericardial effusion are diverse and often stem from various underlying medical conditions, with abnormal fluid production primarily linked to injury or insult to the pericardium, such as pericarditis. The etiology can vary, including inflammatory, infectious, malignant, autoimmune processes, and other less common factors. This can explain as below:
- Often relates to a lack of extensive diagnostic evaluation.
- Human immunodeficiency virus (HIV) infection and viral etiologies (coxsackievirus, hepatitis).
- Secondary bacterial, opportunistic, and malignancy-related mechanisms.
- Involvement through direct extension, retrograde extension, or hematologic seeding.
- Prevalent in lung, breast, leukemia/lymphoma, malignant melanoma, and mesothelioma.
- Postoperative/Postprocedural:
- Common after cardiac surgery, associated with factors like preoperative anticoagulants, valve surgery, and female sex.
- Early chest tube removal may increase the risk of effusions.
- Other Less Common Causes:
- Uremia, myxedema, severe pulmonary hypertension, radiation therapy, acute myocardial infarction, aortic dissection, trauma, hyperlipidemia, chylopericardium, familial Mediterranean fever, Whipple disease, and hypersensitivity or autoimmune-related conditions.
- Drug-associated causes include procainamide, hydralazine, isoniazid, minoxidil, phenytoin, anticoagulants, and methysergide.
Clinical presentation
The key symptoms of pericardial effusion can be categorized as follows:
- Chest pain, pressure, discomfort - Relief is often experienced by sitting up and leaning forward, while exacerbation occurs when lying supine.
- Light-headedness and syncope.
- Palpitations.
- Cough.
- Dyspnea.
- Hoarseness.
- Neurological and Gastrointestinal Symptoms:
- Neurologic manifestations may include anxiety and confusion.
- Hiccoughs may occur as a gastrointestinal (GI) symptom.
Diagnosis
Physical Examination
Cardiovascular Findings:
- Classic Beck Triad of Pericardial Tamponade:
- Hypotension
- Muffled heart sounds
- Jugular venous distention
- Pulsus Paradoxus: Defined as a decrease in systolic blood pressure of more than 10 mm Hg with inspiration, indicating falling cardiac output during inspiration.
- Pericardial Friction Rub:
- High-pitched, scratching, and grating sound, often with up to 3 components per cardiac cycle.
- Heard most frequently during expiration with the patient upright and leaning forward.
- May require firm pressure with the diaphragm of the stethoscope applied to the chest wall at the left lower sternal border.
- Tachycardia.
- Hepatojugular Reflux: Rise in jugular venous pressure (JVP) of greater than 3 cm H2O for more than 30 seconds with pressure applied to the periumbilical region, suggesting elevated central venous pressure.
Respiratory Findings:
- Tachypnea.
- Decreased breath sounds: Secondary to pleural effusions.
- Ewart Sign: Dullness to percussion beneath the angle of the left scapula from compression of the left lung by pericardial fluid.
Additional Findings:
- Hepatosplenomegaly represents a gastrointestinal symptom of pericardial effusion.
- Extremity findings may include weakened peripheral pulses, edema, and cyanosis.
Workup
Lab Studies
- Basic Metabolic Panel: Electrolytes are assessed for metabolic abnormalities, especially in cases of renal failure.
- Complete Blood Count (CBC) with Differential:
- Leukocytosis is checked for evidence of infection.
- Cytopenias may indicate underlying chronic diseases like cancer or HIV.
- Troponin levels may be minimally elevated in acute pericarditis but typically return to normal within 1-2 weeks and are not associated with a worse prognosis.
- Inflammatory Markers: Erythrocyte sedimentation rate and C-Reactive protein help assess the need for anti-inflammatory agents, particularly in recurrent effusions.
- Thyroid-Stimulating Hormone (TSH): Screen for hypothyroidism.
- Blood Cultures: Recommended in the presence of systemic inflammatory response syndrome (SIRS) or fever.
- Rheumatologic Markers: Rheumatoid factor, immunoglobulin complexes, ANA, and complement levels (diminished) are checked in suspected rheumatologic causes.
- Infectious Disease Testing: Specific tests based on clinical suspicion, such as tuberculin skin testing, rickettsial antibodies, and HIV serology.
Pericardial Fluid Analysis:
- Biochemical and cell-count analysis has a low yield in diagnosing the cause.
- Gram stain and culture are crucial for identifying etiology.
- Light Criteria for Exudative Effusion:
- Total protein fluid-to-serum ratio >0.5, LDH fluid-to-serum ratio >0.6, LDH fluid level exceeds two-thirds of the upper limit of normal serum level.
- Specific gravity >1.015, total protein >3.0 mg/dL, LDH >300 U/dL, glucose fluid-to-serum ratio <1.
- Elevated leukocytes (>10,000) with neutrophil predominance suggest bacterial or rheumatic causes.
- Viral cultures, adenosine deaminase, PCR, culture for tuberculosis, smear for acid-fast bacilli in suspected tuberculosis infection, especially in patients with HIV.
- Elevated CEA levels in pericardial fluid have high specificity for malignant effusion.
Pericardial Biopsy:
Considered, especially in cases of suspected malignant pericardial effusion, and may be more diagnostic when combined with pericardioscopy.
Chest X-ray
- Limited sensitivity and specificity for pericardial effusion.
- Chronic effusions may present with a boot-shaped heart or a "water bottle sign," but these findings lack specificity.
- Pulmonary edema, pulmonary vessel engorgement, and pleural effusions may be observed but are not specific to pericardial effusion.
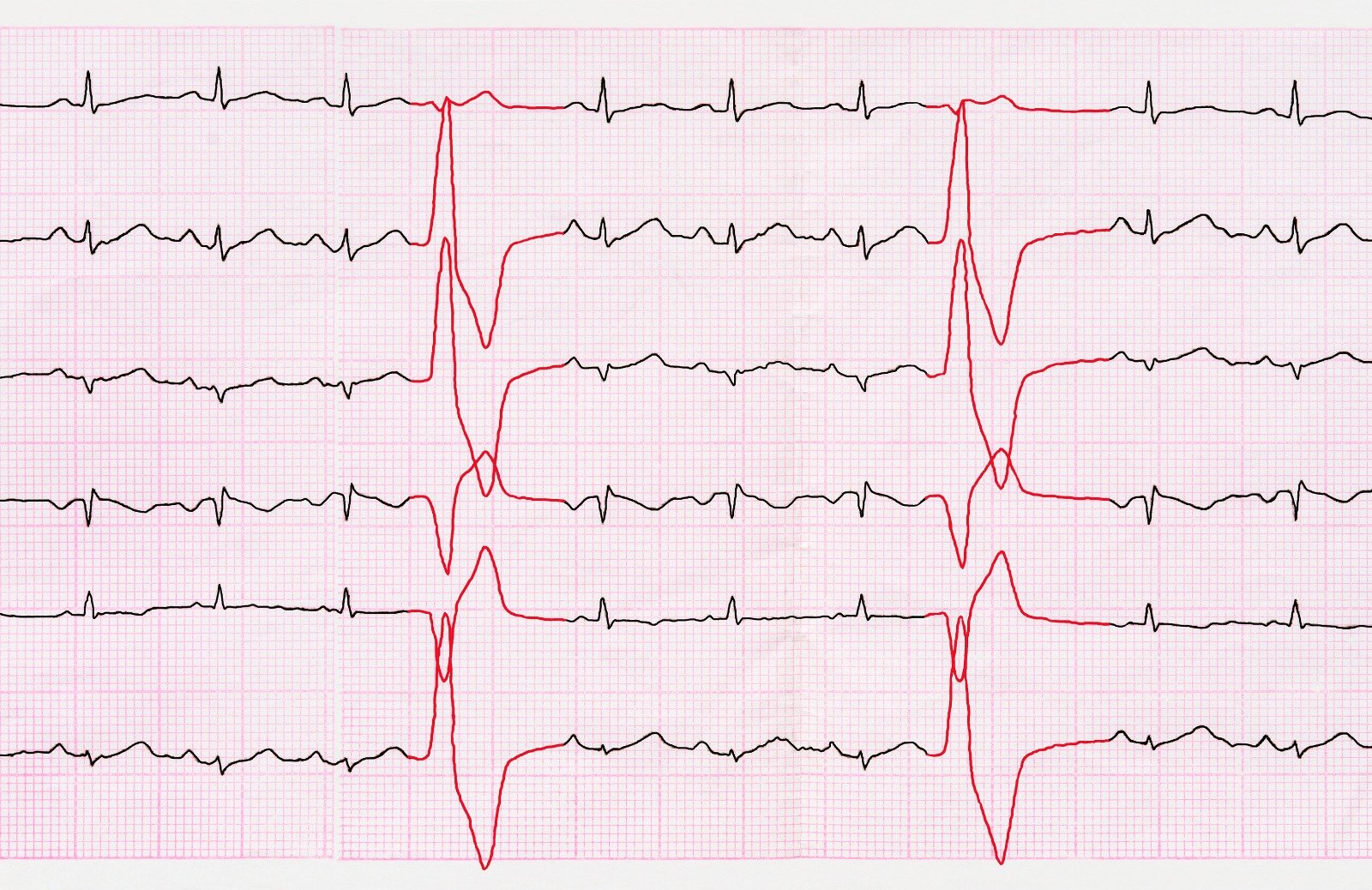
ECG
- Varied findings from normal to non-specific ST-segment changes in small effusions.
- Electrical alternans, a specific but not sensitive finding, may be present in large effusions or tamponade.
- Pericarditis-related ECG changes include PR depressions or diffuse ST elevations.
Echocardiography (TTE or TEE)
- Diagnostic modality of choice for pericardial effusion.
- Provides dynamic assessment, quantification of effusion size, and identification of cardiac tamponade physiology.
- Anechoic fluid surrounding the heart is indicative of pericardial effusion.
- Various echo findings, such as right atrial free-wall collapse, right ventricular free-wall collapse, and increased flow across valves, may suggest pericardial tamponade.
CT/MRI
- Can identify pericardial effusion but is not the preferred diagnostic modality.
- Used when other imaging methods are inconclusive or when additional information is needed.
Treatment & Management
The comprehensive approach to pericardial effusion encompasses various pharmacotherapies, procedural interventions, and management strategies tailored to the specific characteristics and clinical status of each patient.
Management Approaches:
- Symptomatic or tamponade patients require emergent ICU admission.
- Pericardial catheter removal within 24-48 hours to prevent infection.
- Patients educated on symptoms of increasing effusion; regular evaluations recommended.
- Indications for echocardiography: follow-up, large or rapidly accumulating effusions.
Pharmacotherapy:
- Effective for acute idiopathic or viral pericarditis.
- Ibuprofen is preferred for its low adverse effects and favorable impact on coronary blood flow.
- Combined with conventional therapy, reduces symptoms and recurrence.
- Demonstrated effectiveness in the COPE trial.
- Considered recurrent pericarditis unresponsive to NSAIDs and colchicine.
- Associated with an increased risk of relapse; reserved for specific cases.
- Used in purulent pericarditis, requiring urgent drainage and IV antibacterial therapy.
- Tuberculous pericarditis treated with multidrug therapy; surgical resection for constrictive pericarditis.
Procedures:
- Diagnostic and therapeutic; guided by fluoroscopy, echocardiography, or CT.
- Complications include ventricular rupture, dysrhythmias, pneumothorax; recurrence rates up to 90% in cancer patients.
- Pericardiotomy and Pericardiostomy:
- Balloon pericardotomy for recurrent effusions; CT-guided pericardiostomy for challenging cases.
- Subxiphoid pericardial window with pericardiostomy as a low-morbidity alternative.
- Thoracotomy and Median Sternotomy:
- Reserved for cases unresponsive to conservative approaches or with constrictive pericarditis.
- Thoracotomy requires general anesthesia and has higher morbidity; median sternotomy for constrictive pericarditis.
- Video-Assisted Thoracic Surgery (VATS):
- Allows wider pericardial resection than subxiphoid approach.
- Useful for concomitant pleural pathology; requires general anesthesia with single lung ventilation.
References:
- Facp, W. J. S. D. (n.d.). Pericardial Effusion: Practice Essentials, Background, Pathophysiology. https://emedicine.medscape.com/article/157325
- Willner, D. A. (2023, February 20). Pericardial Effusion. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK431089/
- Pericardial effusion: Approach to diagnosis. (n.d.). UpToDate. Retrieved December 26, 2023, from https://www.uptodate.com/contents/pericardial-effusion-approach-to-diagnosis
- Pericardial effusion: Approach to management. (n.d.). UpToDate. Retrieved December 26, 2023, from https://www.uptodate.com/contents/pericardial-effusion-approach-to-management


.webp)
.webp)
.webp)





.webp)

.webp)



.webp)