Introduction
Tetralogy of Fallot (TOF) is a significant congenital heart disorder, impacting blood flow and causing inadequate oxygenation in the lungs, resulting in a right-to-left shunt.
Tetralogy of Fallot distinguished by key features include pulmonary artery stenosis, intraventricular communication, rightward deviation of the aorta's origin, and concentric right ventricular hypertrophy.
Newborns with TOF typically display cyanosis shortly after birth, leading to early medical attention. However, in some instances, cyanosis may only become apparent a few weeks or months after birth. Notably, infants with transposition of the great vessels often manifest cyanosis immediately after delivery.
Anatomy
The exact embryologic abnormality underlying Tetralogy of Fallot (TOF) remains unknown. However, during development, there is an observed anterior and cephalad deviation of the infundibular septum, resulting in a malaligned ventricular septal defect (VSD). The aortic root overrides the defect, leading to subsequent right ventricular outflow obstruction and the development of concentric right ventricular hypertrophy, as depicted in Figure 1. This hypertrophy is believed to be a response to the large VSD and the resultant right ventricular outflow obstruction, resulting in systemic right ventricular systolic pressure.
Ventricular septal defect — The VSD in TOF is predominantly a single, large malaligned subaortic defect located in the perimembranous region of the septum. Rarely, the VSD may extend into the muscular septum.
Right ventricular outflow obstruction — The right ventricular outflow obstruction often occurs at multiple levels, including subvalvar obstruction due to the anterior and cephalad deviation of the infundibular septum. Muscular band hypertrophy can further accentuate subvalvar obstruction, and the pulmonary valve annulus is typically hypoplastic. Additionally, the pulmonary valve itself is frequently bicuspid and stenotic. Supravalvar narrowing in the main pulmonary artery at the sinotubular ridge is not uncommon, and further obstruction may be found at the branch pulmonary arteries, which can be diffusely hypoplastic or have focal areas of stenosis.
Overriding aorta — TOF is characterized by an overriding aorta, a congenital anomaly where the aorta is displaced to the right over the VSD rather than the left ventricle. The degree of aortic override varies, with its measurement being a significant factor in differentiating TOF from double outlet right ventricle.
Associated cardiac features — Approximately 40 percent of patients with TOF exhibit associated cardiac anomalies. These include a right aortic arch in about 25 percent of cases, abnormalities of the coronary arteries (such as the left anterior descending arising from the right coronary artery) in approximately 10 percent, aorticopulmonary collateral vessels that may require attention, and the presence of a patent ductus arteriosus, multiple ventricular defects, complete atrioventricular septal defects, and infrequently, aortic valve regurgitation.
Pathophysiology
In pediatric patients
The pathophysiology of tetralogy of Fallot (TOF) in pediatric patients involves a complex interplay of genetic and prenatal factors. Genetic studies point to potential susceptibility genes such as methylene tetrahydrofolate reductase (MTHFR) and VEGF polymorphisms.
Prenatal factors, including maternal infections, poor nutrition, advanced maternal age, and certain syndromes, contribute to a higher incidence of TOF.
Tetralogy of Fallot is often associated with conotruncal malformations, collectively known as CATCH 22, and cytogenetic analysis may reveal deletions on chromosome 22q11, indicative of DiGeorge syndrome. Hemodynamically, TOF in pediatric patients is characterized by right ventricular outflow tract obstruction, and the severity determines the direction of intracardiac shunting.
In the adult
As patients with TOF transition into adulthood, the pathophysiology evolves, with a focus on the consequences of pulmonary valve insufficiency. Previously considered benign, pulmonary valve insufficiency leads to progressive right ventricular dysfunction and arrhythmias. The resulting RV dilatation, fibrosis, and myocardial damage contribute to decreased exercise endurance and the development of ventricular arrhythmias.
Arrhythmias, both atrial and ventricular, are common in adults with repaired TOF, occurring in 10-35% of cases. Sudden death is a known risk, particularly in individuals with moderate to severe pulmonary valve insufficiency. Notably, the risk of late sudden death is significantly higher in individuals who have undergone TOF surgery compared to their age-matched counterparts.
Clinical Presentation
The clinical presentation of tetralogy of Fallot (TOF) varies between pediatric and adult patients, highlighting the evolving nature of this congenital heart condition.
Pediatric Presentation:
In infants with TOF, feeding difficulties and failure to thrive are common, and cyanosis may become apparent during crying or feeding, leading to potentially life-threatening hypoxic tet spells. Older children may exhibit a characteristic squatting behavior to increase pulmonary blood flow. As they age, exertional dyspnea may worsen, and complications such as hemoptysis may arise. Cyanosis tends to progress with time, demanding surgical intervention. Factors such as acidosis, stress, infection, and exercise can exacerbate cyanosis in these patients.
Adult Presentation:
After corrective surgery in childhood, TOF patients may remain symptom-free for several decades. However, the long-term palliative nature of the surgery becomes evident as RV dysfunction and pulmonary valve insufficiency develop over time. Mild insufficiency may be asymptomatic initially, but as it progresses, patients may experience exercise intolerance, palpitations, and a decline in overall well-being.
Physical examination reveals signs of right heart failure, while auscultation may detect murmurs associated with pulmonary valve insufficiency and residual ventricular septal defects. Arrhythmias become more common, necessitating corrective surgery to address the pulmonary valve.
Long-Term Considerations:
It is crucial to recognize that surgical correction in adulthood does not prevent ongoing anatomic changes in the right ventricle and pulmonary vessels. Therefore, the majority of adults with repaired TOF eventually present with symptoms related to RV dysfunction and right ventricular outflow tract obstruction.
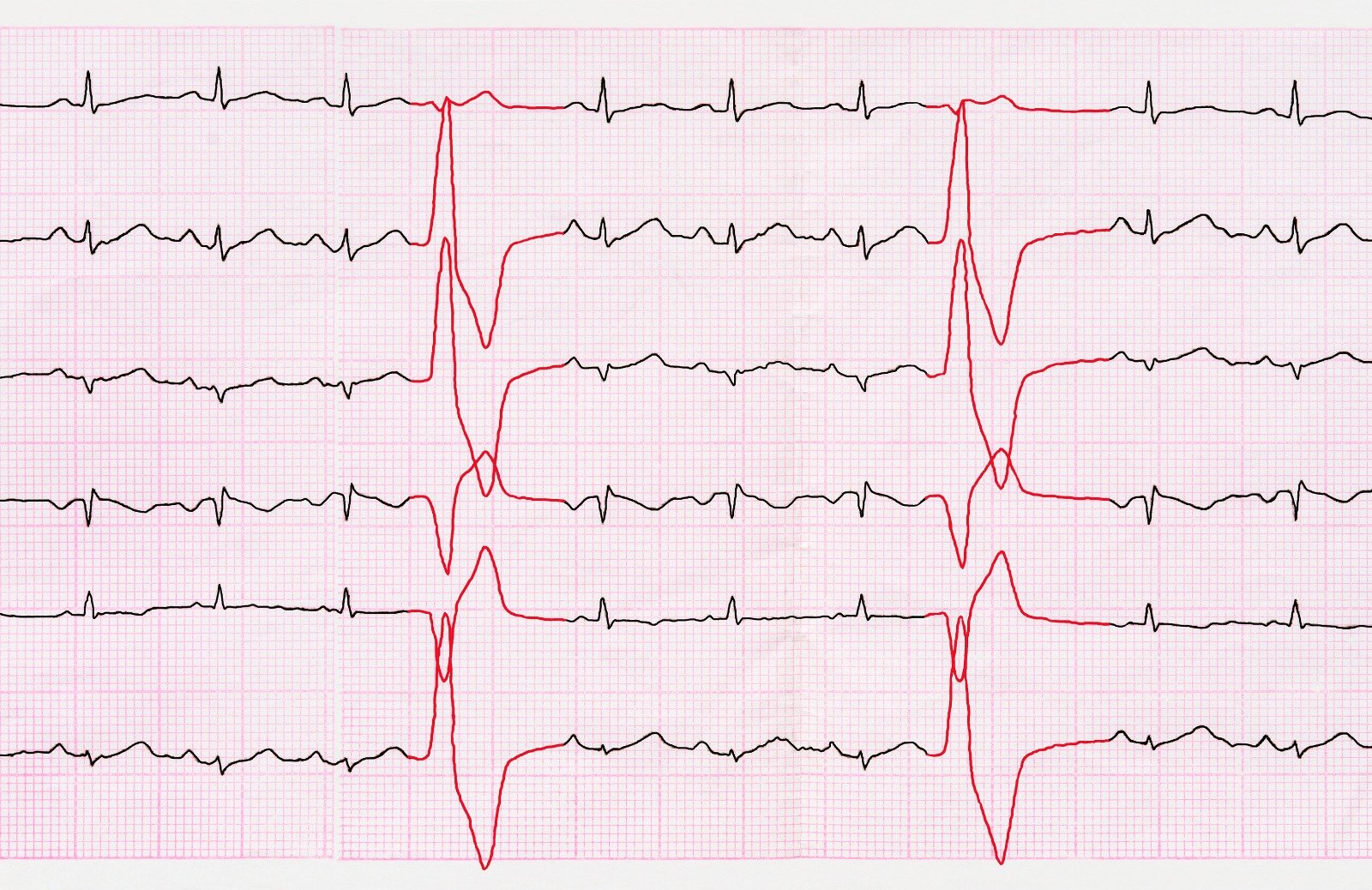
Diagnosis
The primary method of diagnosis involves the use of echocardiography, with additional examinations such as electrocardiogram and chest radiography also employed. In certain cases, cardiac catheterization may be deemed necessary to provide a comprehensive assessment of both anatomy and hemodynamics.
Prenatal diagnosis has witnessed significant progress, thanks to advancements in prenatal screening and fetal echocardiography. This enhanced capability in prenatal diagnosis facilitates proactive planning for delivery, particularly in instances where severe cases necessitate the implementation of prostaglandin therapy.
Treatment & Management
Medical Management:
- Severity of right ventricular outflow tract (RVOT) obstruction determines the need for medical intervention.
- Neonates with severe RVOT obstruction may require intravenous prostaglandin therapy.
- Tet spells (hypercyanotic spells) require a step-wise approach, including knee-chest position, oxygen, morphine, fluid bolus, beta-blockers, and phenylephrine.
- Heart failure symptoms may necessitate digoxin and a loop diuretic.
- Antibiotic prophylaxis is recommended until surgical correction for unrepaired cyanotic congenital heart disease.
Surgical Management:
- Most patients with Tetralogy of Fallot (TOF) undergo intracardiac repair by one year of age.
- Surgical goals include relieving RVOT obstruction, separating pulmonary and systemic circulations, preserving right ventricular function, and minimizing post-procedure pulmonary valve issues.
- Primary intracardiac repair is the preferred treatment, involving patch closure of the ventricular septal defect (VSD) and enlargement of the RVOT.
- Surgical approaches aim to maintain pulmonary valve competence, with a "valve sparing approach" when feasible.
- Transannular patch repair is the most common strategy, and alternative procedures involve valved conduits or monocusp valves.
- Historical two-staged procedures (palliative shunt followed by intracardiac repair) are now mostly replaced by primary intracardiac repair.
References:
- Bhimji, S. (n.d.). Tetralogy of Fallot (TOF) in Adults: Practice Essentials, Background, Anatomy. https://emedicine.medscape.com/article/2035949
- Tetralogy of Fallot (TOF): Pathophysiology, clinical features, and diagnosis. (n.d.). UpToDate. Retrieved December 20, 2023, from https://www.uptodate.com/contents/tetralogy-of-fallot-tof-pathophysiology-clinical-features-and-diagnosis
- Tetralogy of Fallot (TOF): Management and outcome. (n.d.). UpToDate. Retrieved December 20, 2023, from https://www.uptodate.com/contents/tetralogy-of-fallot-tof-management-and-outcome



.webp)
.webp)


.webp)



.webp)
.webp)



.webp)