Supraventricular tachyarrhythmia is a cardiac condition where the heartbeat rate is suddenly elevated, which may be associated with chest pain, dyspnea, and fainting. It may last for a very short time and resolve spontaneously, or it may persist or be frequently recurrent. The management of supraventricular tachyarrhythmia is dependent on the underlying pathophysiology of arrhythmia, the severity of symptoms, and the recurrence of episodes.
Acute Management (based on ACC/AHA/HRS Recommendations)
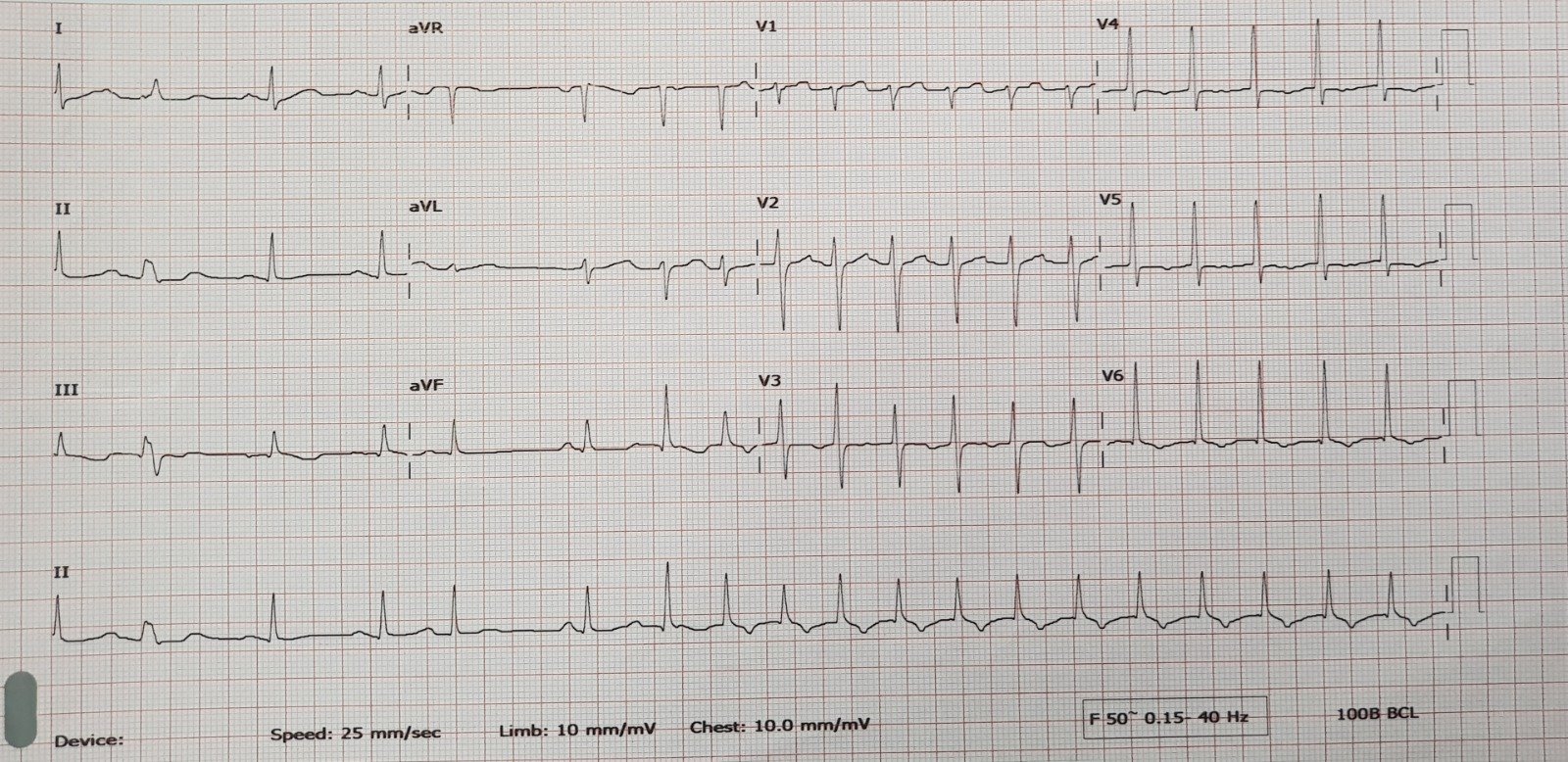
Continuous electrocardiography (ECG) must be performed during the management of acute supraventricular tachyarrhythmia.
-
Vagal Maneuver while the patient is lying down
It is recommended as an initial management plan. It includes:
- Coughing.
- Valsalva Maneuver a patient in a supine or semirecumbent position takes a normal breath and then vigorously exhales the air for 10-15seconds while the nose and mouth are closed. A modified Valsalva has added 15 seconds of leg elevation at 45 degrees while in the supine position after initial bearing down in a semirecumbent position.
- Carotid sinus massage while raising the chin for 5-10 seconds, unless the patient is diagnosed with carotid stenosis or a recent transient ischemic attack or stroke.
- The diving reflex involves applying a wet, ice-cold towel to the face or immersing the face in 10°C water for 20-30 seconds.

It is recommended for initial management but must be used with caution in cases of antidromic atrioventricular reentrant tachycardia (AVRT), as it may lead to the development of atrial fibrillation with rapid ventricular rate.
It is administered through an intravenous route near the heart in an initial 6mg dose that can be followed by a 12 mg dose if the response is insufficient within 2 minutes, then repeated with a further 12 mg dose if needed, and each dose must be followed with a flush with normal saline to ensure that the dose reaches the heart directly since adenosine is rapidly metabolized and its half-life is less than 10 seconds.
-
Non-Dihydropyridine Calcium Channel Blockers or Beta Blockers
They can be used for stable patients if they are nonresponsive to initial management.
Diltiazem is administered as a bolus dose of 0.25 mg/kg over 2 minutes, followed by an infusion of 5–15 mg/hr.
Verapamil is administered as an initial bolus dose of 5–10 mg over 2 minutes, with a repeated 10mg dose after 30 minutes if the response is inadequate, and then an infusion with 0.005 mg/kg/min can be initiated.
Esmolol is administered as a bolus dose of 500 mg/kg over a minute, followed by an infusion of 50-300 mcg/kg/min, and the bolus dose must be repeated if the infusion rate is increased.
Metoprolol Tartrate is administered as a bolus dose of 2.5–5 mg over 2 minutes, which can be repeated over 10 minutes up to 3doses
Propranolol is administered as a bolus dose of 1mg over a minute, which can be repeated every 2 minutes up to 3 doses.
It can be used if initial pharmacological management has failed or is contraindicated for use, and the underlying pathophysiology of supraventricular tachyarrhythmia is related to atrioventricular nodal reentrant tachycardia (AVNRT) or focal atrial tachycardia.
Amiodarone is administered as a bolus dose of 150mg over 10 minutes, which is followed by an infusion at a rate of 1mg/min for 6 hours, then the rate is reduced to 0.5 mg/min for an additional 18 hours.
-
Intravenous Ibutilide or Procainamide
Antiarrhythmic medications can be used in stable patients with atrial fibrillation associated with pre-excitation and antidromic atrioventricular reentrant tachycardia (AVRT). Since atrioventricular nodal blocking agents such as non-dihydropyridine CCB, beta-blockers, intravenous digoxin, and intravenous amiodarone may be harmful in this case as atrioventricular node conduction is so slow.
-
Synchronized Direct Current (DC) Cardioversion
It is recommended if initial pharmacological management has failed or if the patient is hemodynamically unstable.
- Any defined predisposing factor must be eliminated, such as caffeine, nicotine, and uncontrolled hyperthyroidism.
- Wide QRS complex tachycardia with unknown origin must be managed as ventricular tachycardia.
Chronic Management
Long-term therapeutic management may be indicated for some patients with recurrent supraventricular tachycardia episodes.
-
Pharmacological medications
They may be used to control symptoms until definite management with catheter ablation is performed, unless it is contraindicated.
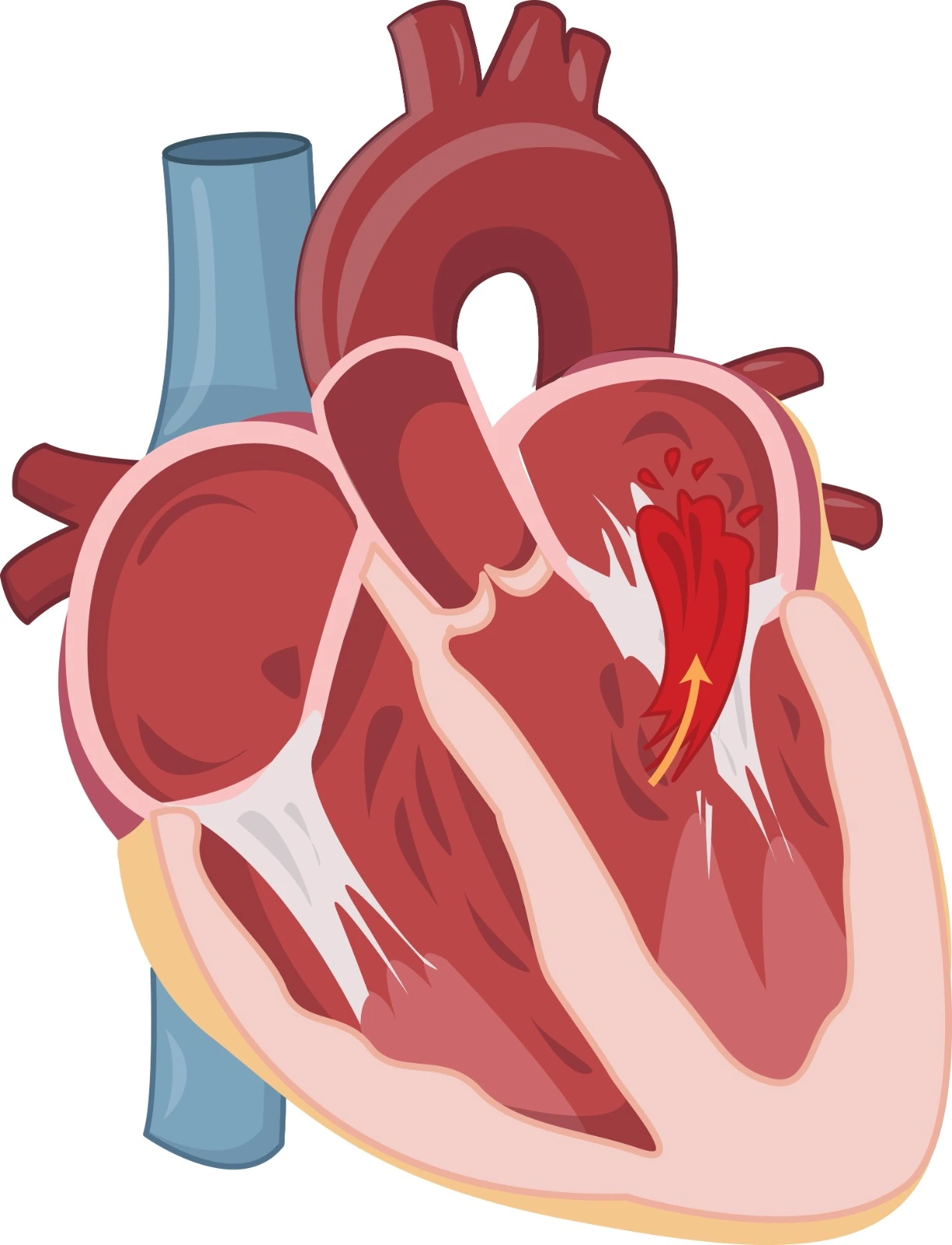
It is a procedure to destroy cells with a slow electrical pathway in the case of atrioventricular nodal reentrant tachycardia (AVNRT) or a re-entry pathway in the case of atrioventricular reentrant tachycardia (AVRT) and Wolf Parkinson White syndrome (WPWS).
References

.webp)
.webp)
.webp)
.webp)
.webp)

.webp)