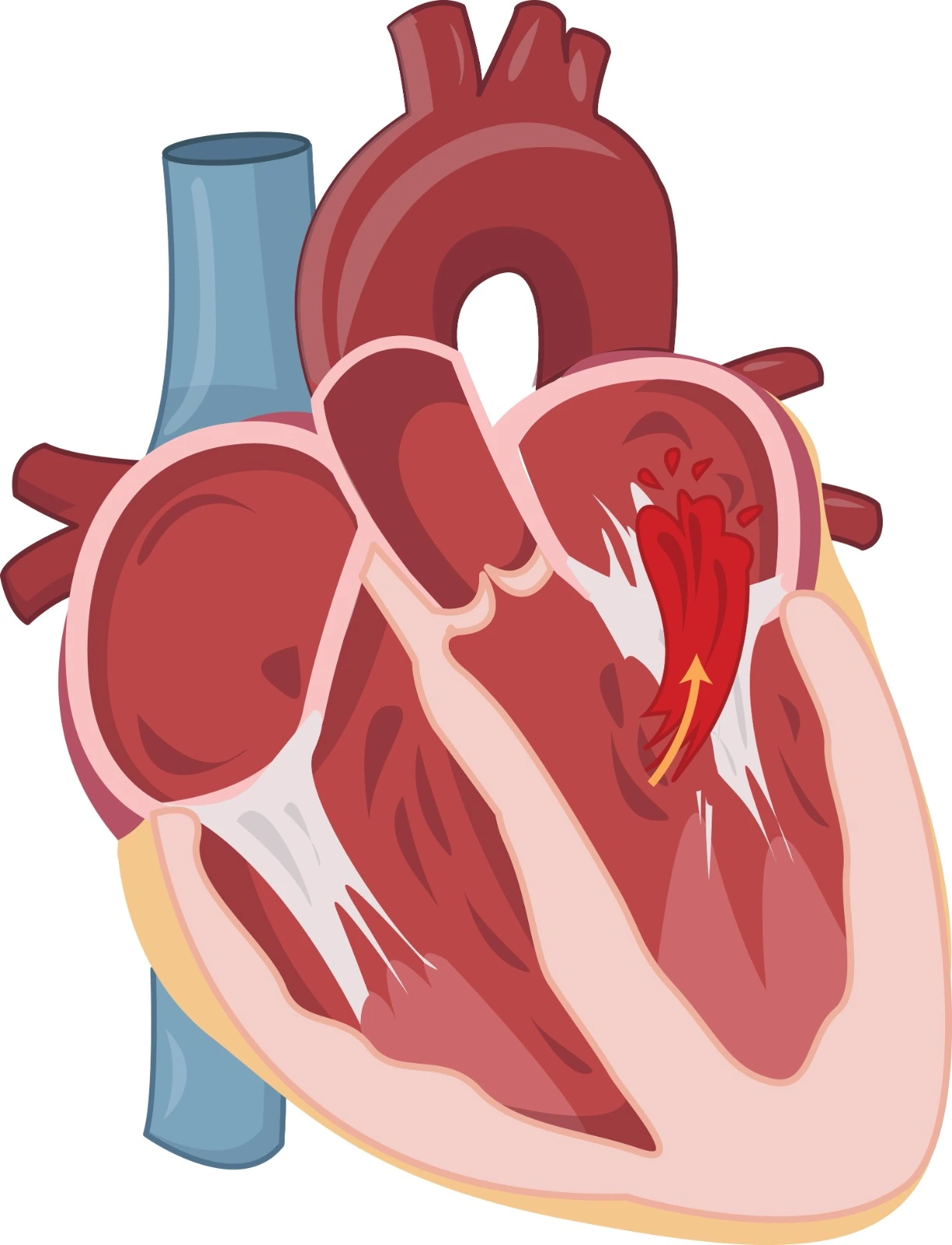
Heart failure is one of the most common heart diseases worldwide. It affects patients' quality of life and increases the risk of hospitalization and mortality. Systolic Heart Failure is defined as a structural or functional impairment in the filling or ejection of blood from the left ventricle, which pumps oxygen-rich blood from the lungs to the rest of the body. Since the left ventricle is larger than the other chambers, it supplies most of the heart's pumping power. In the condition of systolic heart failure, the left ventricle loses its ability to contract normally, resulting in insufficient blood being pushed into circulation. The percentage of blood the left ventricle pumps out with every beat becomes lower, causing the ejection fraction to be less than 40%, whereas in normal conditions, it ranges between 55% and 70%. As a result, the left side of the heart must work harder to pump the same amount of blood.
Medications for systolic heart failure
Diuretics for Managing Congestion
Loop diuretics, mainly Furosemide, are the drug of choice. They have the highest water elimination effect by inhibiting the Na-K-2Cl channel at the thick ascending loop of Henle, which is associated with the highest Na reabsorption fraction. Loop diuretics preserve their diuretic effect even in cases of renal dysfunction.
Daily fluid input-output should be 2L (1L in cases of renal impairment). Diuretic resistance can be managed by increasing the dose (up to a maximum of 600mg daily), extending the infusion, or adding a thiazide diuretic if the glomerular filtration rate (GFR) is greater than 30.
Medications with mortality-morbidity benefit unless contraindicated:
- ACEI or ARB or ARNI
- ACEI (Angiotensin-Converting Enzyme Inhibitor):
ACEIs are vasodilators that reduce preload and afterload while preventing cardiac remodeling. They achieve this by inhibiting the angiotensin-converting enzyme, which normally converts Angiotensin1 to Angiotensin2.
Angiotensin2, when not inhibited, has vasoconstrictive effects, enhances aldosterone's effects (leading to sodium and water retention), and stimulates ADH secretion (antidiuretic hormone).
It's worth noting that ACEIs are associated with an increased risk of angioedema and dry cough, which is a result of bradykinin accumulation. Additionally, they can contribute to acute kidney injury (AKI) by dilating the renal efferent arterioles, which reduces the glomerular filtration rate (GFR).
- ARB (Angiotensin II Receptor Blocker):
ARBs work by inhibiting Angiotensin2 receptors. They are typically used in cases where angioedema develops following ACEI use but with a recommended 6-week interval or when dry cough occurs with ACEIs.
- ARNI (Angiotensin Receptor Neprilysin Inhibitor): Sacubitril-Valsartan
Sacubitril-Valsartan is an ARNI. Sacubitril, a prodrug of Sacubitrolate, inhibits the neprilysin enzyme, which typically degrades Atrial and Brain Natriuretic Peptides, Angiotensin2, and Bradykinin. The accumulation of AMP and BNP due to neprilysin inhibition results in vasodilation, diuresis, natriuresis, and renin inhibition effects.
ARNIs are typically combined with ARBs to prevent the accumulated effects of Angiotenin2. They are not combined with ACEIs, as ACEIs can exaggerate bradykinin accumulation.
When transitioning from ACEIs to ARNIs, it is recommended to have a 36-hour interval to avoid cough.
It's important to note that all of these medications are contraindicated in pregnancy, hyperkalemia, and bilateral renal artery stenosis.
Bisoprolol, Carvedilol, and Metoprolol succinate work on the cardiac β1 receptor to reduce heart rate, oxygen demand, inhibit the Renin-Angiotensin-Aldosterone System (RAAS), and prevent heart remodeling.
Nebivolol is employed based on European guidelines and has a vasodilation effect.
- Mineralocorticoid receptor antagonist: Spironolactone, Eplerenone
Mineralocorticoid receptor antagonists reduce fluid retention, lower blood volume, and prevent harmful cardiac remodeling, thereby improving systolic heart failure.
These medications, including Spironolactone and Eplerenone, are contraindicated in individuals with hyperkalemia and a glomerular filtration rate (GFR) of less than 30.
- SGLT2 Inhibitors: Dapagliflozin, Empagliflozin
These medications, including Dapagliflozin and Empagliflozin, work by inhibiting the renal reabsorption of glucose and sodium.
- Isosorbide dinitrate-Hydralazine
Isosorbide dinitrate-hydralazine reduces afterload, enhances blood flow, alleviates symptoms, and reduces mortality in systolic heart failure. It can be prescribed for African-American patients.
Ivabradine is a sinus node modulator used to lower heart rate when ejection fraction (EF) is below 30% and the resting heart rate is above 70 bpm despite maximum tolerated beta-blockers.
Consider the addition of:
- Digoxin: Digoxin is an ATPase inhibitor with positive inotropic effects (increasing heart contraction) and negative chronotropic activity (reducing heart rate). It is used in symptomatic patients to reduce hospitalizations.
- Soluble guanylate cyclase: Vericigut increases cGMP as a vasodilator and reduces heart remodeling when conditions worsen despite adequate management, recent hospitalization, or IV diuretic use with BNP levels exceeding 300 or proBNP exceeding 100.
- Anticoagulants for DVT Prophylaxis and Treatment
- Potassium Binders for Hyperkalemia
Reference:


.webp)
.webp)
.webp)
.webp)
.webp)

.webp)