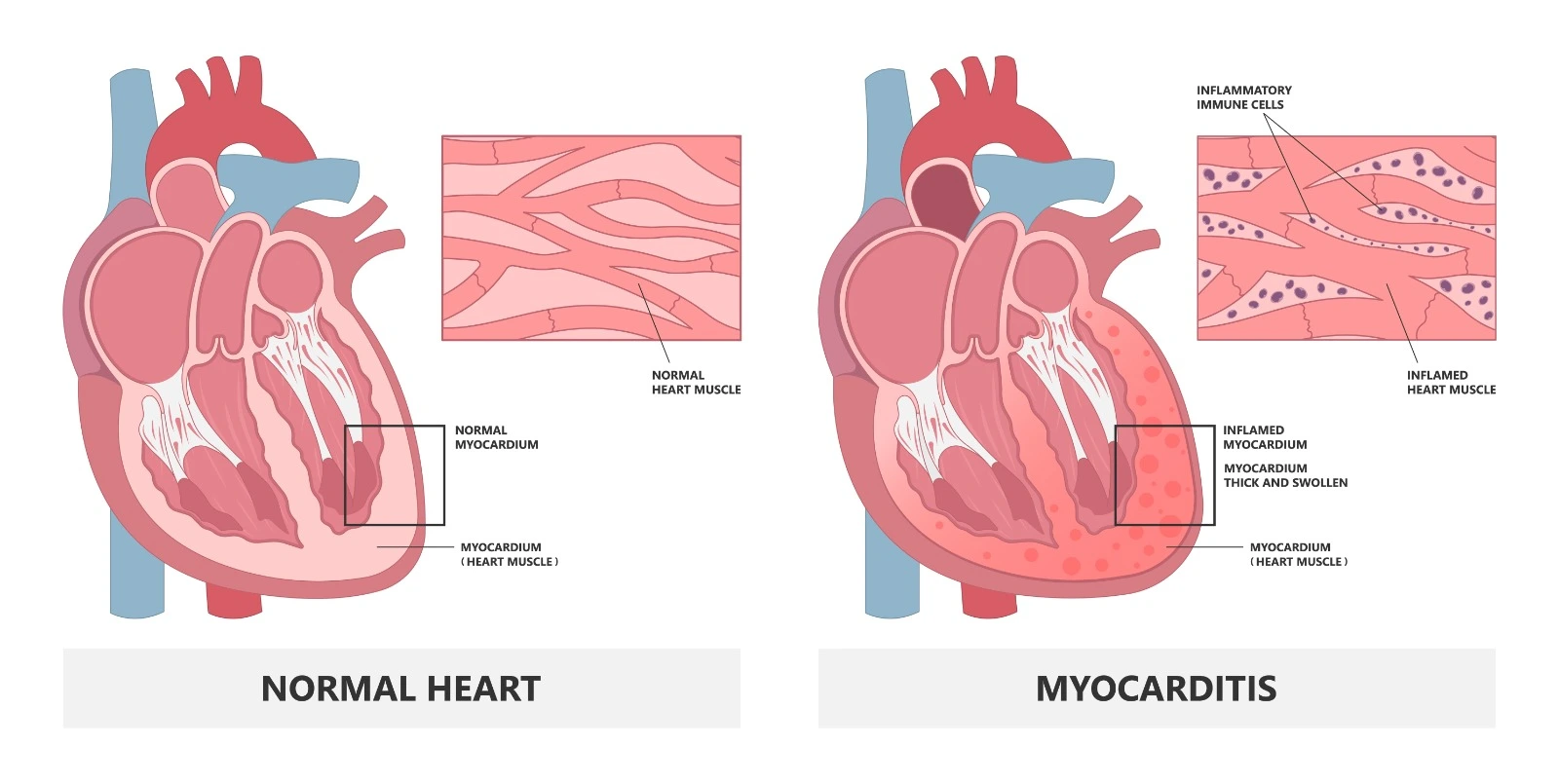
The myocardium is the middle layer of the heart wall; it is thought to be the thickest layer in the heart wall, particularly at the ventricles. It is a muscular layer of unique striated cardiomyocytes that is responsible for heart contractions. It also contains the Sinoatrial Node, the pacemaker of the heart. It receives nourishment from epicardium coronary arteries and is innervated by the Accelerans and Vagus nerves. Several factors may cause inflammation in the myocardium, which may result in clinical symptoms and cardiac complications.
Pathophysiology
Myocarditis is an inflammation of the myocardial layer that is caused by infectious microorganisms or autoimmune diseases that are cytotoxic in nature and induce apoptosis upon cytokine release from activation of secondary immune reactions. This typically happens during the acute phase, which lasts for the first two weeks. After that, human leukocyte antigen (HLA) is present in the myocardium along with the viral genome if it’s the causative agent, so the autoimmune reaction is the main process during the chronic phase.
Although the underlying cause of myocarditis is considered idiopathic in more than 50% of cases, many other causes may be involved:
- Viral infection is considered a major factor, such as adenovirus, influenza, cytomegalovirus, Epstein-Barr virus, HIV-1, viral hepatitis, varicella, and herpes simplex virus.
- Bacterial infections, such as Streptococci, Staphylococcus, Meningococcal, Mycoplasma pneumoniae, and Tuberculosis
- Fungal infections such as Candidiasis, Aspergillosis, and Cryptococcosis
- Protozoal infections such as toxoplasmosis, malaria, and leishmaniasis
- Peripartum Cardiomyopathy
- Post-organ transplant rejection
- Chronic inflammatory diseases, such as giant cell myocarditis, systemic lupus erythematosus, Irritable bowel diseases, thyrotoxicosis, rheumatoid arthritis, and sarcoidosis
- Iatrogenic: Chemotherapies, Penicillin, Sulfonamides, Methyldopa, Spironolactone, Phenytoin, Carbamazepine, Stimulants, Carbon Monoxide, and Mercury
Classification
Myocardial classification based on histological findings:
- Lymphocytic Myocarditis is the most common type and is associated with viral infections.
- Giant cell Myocarditis is associated with a sudden, severe presentation and the highest risk.
- Eosinophilic Myocarditis is associated with hypersensitivity reactions.
- Granulomatous Myocarditis is associated with cardiac sarcoidosis.
Myocarditis is also classified into:
- Fulminant myocarditis: early symptoms are similar to those of a viral infection, which rapidly affects the larger myocardial area and leads to ventricular dysfunction and cardiovascular shock. It is associated with a high mortality risk.
- Acute myocarditis: early symptoms are less distinct but also associated with ventricular dysfunction, which may progress to dilated cardiomyopathy.
- Chronic active myocarditis, where symptoms develop slowly along with chronic inflammatory changes, ventricular dysfunction, and frequent relapses
- Chronic persistent myocarditis is a slowly progressive disease with ongoing myocyte infiltration and necrosis but without ventricular dysfunction.
Clinical presentation
Patient presentation is variable based on the underlying cause, current disease phase, and disease progression. Acute myocarditis usually develops within three months, while chronic myocarditis usually develops over an extended period of more than three months.
Patients with acute myocarditis may present with:
- Acute chest pain developed within one to four weeks post-infection. It may be associated with troponin elevation and ischemic electrocardiogram changes but without any evidence of coronary artery disease upon angiography.
- New presentation or worsening of established heart failure within two weeks to three months.
- Patients may present with life-threatening arrhythmias or cardiogenic shock. In addition to sudden cardiac death,
Diagnostic considerations
- A physical examination may detect complications of myocarditis rather than the disease itself. Patients with heart failure may have edema, elevated jugular vein pressure, a third heart sound, and valvular murmurs.
- Laboratory tests may reveal elevated acute-phase reactants such as C-reactive protein during acute myocarditis.
- Beta-natriuretic peptide is a cardiac biomarker that can be used for the screening and diagnosis of heart failure.
- Troponin is a cardiac biomarker that is usually elevated in acute myocarditis but can't be used for exclusion, and its chronic elevation is associated with ongoing myocardium necrosis.
- An electrocardiogram can detect ischemic heart conditions and arrhythmias.
- A chest X-ray can identify any pulmonary congestion.
- An echocardiogram is used to identify any structural changes in heart chambers and access ventricular and valvular function.
References


.webp)
.webp)


.webp)



.webp)

.webp)



.webp)