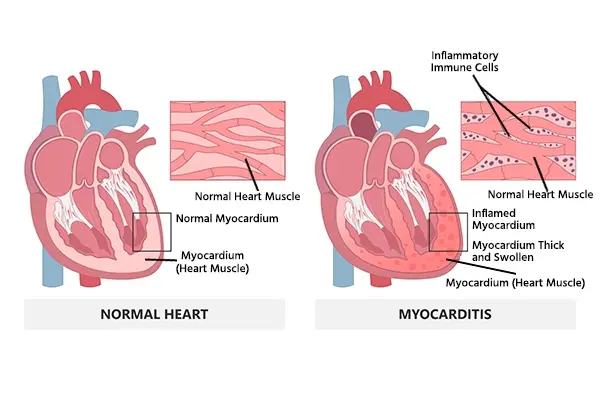
Infections, inflammatory conditions, and medications may cause inflammation of the muscular layer of the heart and the development of myocarditis. Myocarditis may be associated with many clinical symptoms, such as chest pain and palpitations. In addition, it affects cardiac contractility and blood circulation and could lead to heart failure, arrhythmia, stroke, myocardial infarction, and sudden cardiac death.
Myocarditis may be prevented by immune boosting through getting vaccine shots up to date, frequent hand washing, and avoiding direct contact with ill people. Myocarditis may be self-limited and doesn’t require treatment, while the management of other cases must be based on clinical symptoms and the underlying cause to stabilize the patient and improve cardiac function.
Indication for Hospitalization
It is indicated for all patients with acute myocarditis to monitor the patient for at least 48 hours through electrocardiography, echocardiography, and cardiac biomarker tests. Some patients may need advanced treatment and invasive monitoring.
Non-Pharmacological Recommendations
- High-intensity physical activities may be associated with negative outcomes. Competitive sports activities must be prohibited for at least 3-6 months if heart failure develops as a result of myocarditis, with frequent monitoring using a Holter monitor, exercise electrocardiogram, and echocardiography.
- Alcohol consumption must be minimized, as it may worsen myocarditis.
Pharmacological Therapy
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are not effective for myocarditis management and must be avoided in heart failure.
- Corticosteroids may be indicated for the management of viral or eosinophilic myocarditis. In addition, methylprednisolone 1000mg IV is indicated before biopsy if immune-mediated fulminant is suspected. While they are contraindicated in heart failure and arrhythmic patients.
- Anticoagulants are indicated if systemic embolism or a left ventricular thrombus is identified or if atrial fibrillation is diagnosed in heart failure patients.
- Amiodarone or ibutilide may be indicated for the management of symptomatic sustained supraventricular arrhythmia, symptomatic nonsustained ventricular arrhythmia, and recurrent ventricular arrhythmia. While other antiarrhythmic agents in classes I and III must be avoided due to negative ionotropic effects and proarrhythmic risks,
- Digoxin efficacy and safety are not well established for the management of arrhythmia in patients with myocarditis, so it is recommended to be avoided.
- Calcium Channel Blockers must be used with caution for Arrhythmia in patients diagnosed with Heart Failure
- Diuretics, Sodium-Glucose Cotransporter 2 (SGLT2) inhibitors, Beta-blockers, Mineralocorticoid receptor antagonists (MRA), and Angiotensin Receptor-Neprilysin Inhibitor (ARNI) or Angiotensin Converting Enzyme Inhibitors (ACEI) or Angiotensin2 receptor blockers (ARB) are indicated for hemodynamically stable patients if systolic heart failure is diagnosed.
- Dobutamine may be indicated in congested patients with fulminant myocarditis.
- Intravenous positive Ionotropic and vasopressor agents, such as norepinephrine and epinephrine, can be used to manage cardiogenic shock by improving cardiac contractility and are indicated for the management of fulminant myocarditis.
- Immunosuppressive therapy may be indicated for severe, complicated cases with underlying autoimmune or chronic inflammatory disorders.
Mechanical Circulatory Support Measurements
- A pacemaker may be indicated for patients with Bradycardia or heart block during acute myocarditis.
- Biventricular pacing is indicated for the management of giant cell myocarditis (GCM) that leads to right and left ventricular dysfunction.
- Urgent cardioversion is indicated for the management of sustained ventricular arrhythmia.
- An implantable cardioverter defibrillator (ICD) may be indicated for the management of ventricular arrhythmia or syncope in patients with chronic myocarditis with reduced ejection fraction, heart failure, or cardiac arrest if life expectancy is longer than one year.
- An intra-aortic balloon pump can be inserted through a catheter procedure to reduce the pressure on the heart and allow blood circulation to the body.
- A ventricular assist device (VAD) is indicated to aid blood ejection and perfusion to the body in cases of severe heart failure until heart transplantation is convenient.
- Extracorporeal membrane oxygenation (ECMO) can be used in severe heart failure cases to allow sufficient gas exchange through blood circulation in the external machine. It can be used until heart transplantation is possible.
- Heart transplantation may be the definitive treatment for severe chronic myocarditis cases if other measurements have failed to improve cardiac function during the past 30 days in patients with cardiomyopathy and refractory failure. In addition, it may be effective for the management of giant cell myocarditis.
References


.webp)
.webp)


.webp)



.webp)

.webp)



.webp)