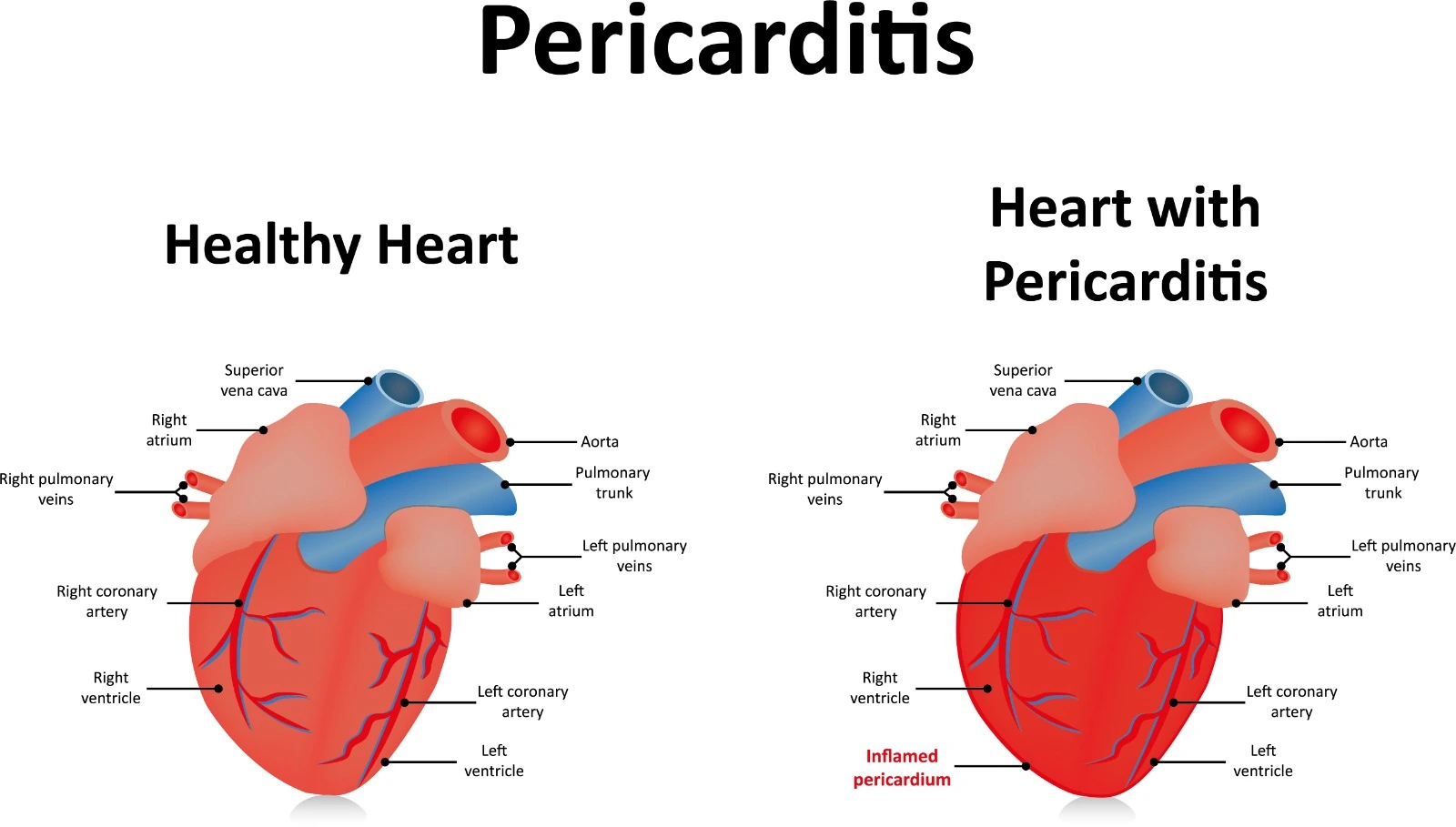
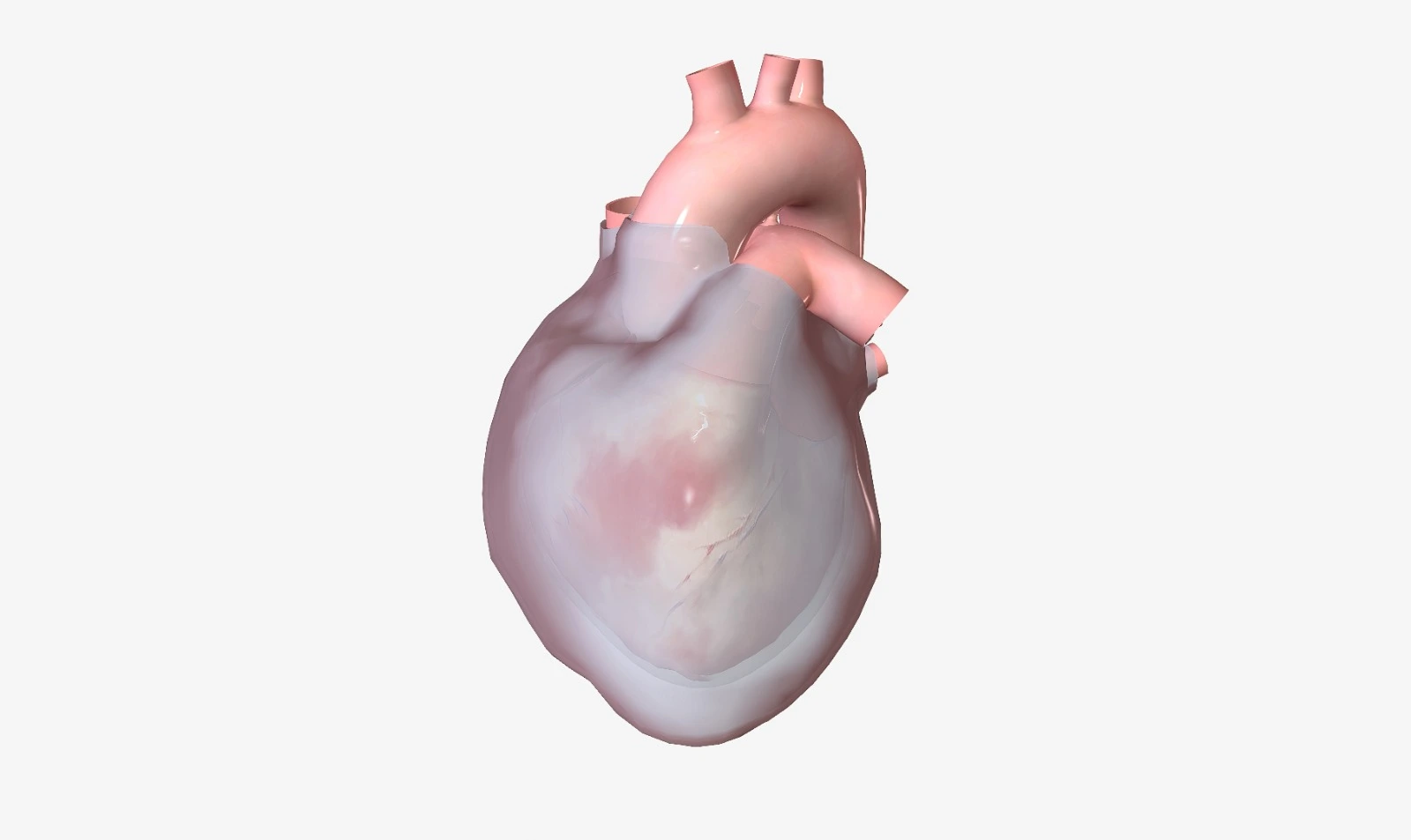
The pericardium consists of multiple layers that surround the heart. It has a major role, as it keeps the heart stable in its place, allowing limited expansion of the heart when needed, prevents friction of the heart with surrounding tissues and organs since the pericardial cavity contains a small amount of lubricating fluids, and protects the heart from outer pressure, invading pathogens and malignancies. The pericardium may get inflamed by many factors, which are associated with multiple symptoms and electrocardiogram changes.
Pathophysiology and Etiology
Acute pericarditis is linked to acute inflammation of the pericardium layers, along with serous or purulent fluid or fibrous material accumulation within the pericardial cavity. Moreover, idiosyncratic pericarditis is associated with a significant number of cases.
Acute pericarditis may be associated with pericardial effusion and cardiac tamponade and may develop into constrictive pericarditis.
It is considered non-pathogenic and caused by chronic inflammatory disorders such as rheumatoid arthritis and systemic lupus erythematosus.
It is the most common cause of acute pericarditis. It's associated with acute myocardial infarction (also called myopericarditis), radiation, trauma, and cardiac surgeries. In addition to accumulated uremic metabolic toxins and elevated free radicals in renal failure cases.
- Purulent or Suppurate Pericardial
It is induced by pathological microorganism invasion, which is exacerbated by immunosuppressive conditions. Viruses are the main underlying cause of pathogens, and acute pericarditis may develop from myocarditis. Bacterial infections due to gram-positive, gram-negative, atypical, and anaerobic bacteria may be associated with some acute pericarditis cases. Also, fungal infections are reported to cause acute pericarditis. Pathogen sources may be cardiac, pulmonary, bloodstream, or postoperative.
In this type, blood is detected inside the pericardium. It has occurred with non-infectious inflammatory conditions and trauma. It may also be related to a severe infection, such as bacterial tuberculosis.
Prognosis
The prognosis of acute pericarditis is dependent on the underlying cause. Idiopathic acute pericarditis and viral acute pericarditis are usually associated with a positive prognosis. Whereas, other cases associated with elevated body temperature >38°C, failed initial treatment with nonsteroidal anti-inflammatory drugs, and coexisting large pericardial effusion or Cardia tamponade have a poor prognosis. Purulent pericarditis is associated with a high mortality risk (around 20–30%).
Clinical presentation
Acute pericarditis is more common in adolescent males. Acute pericarditis clinical symptoms are not indistinct. Nevertheless, patients, -especially with infectious pericarditis, usually present with sudden, intense pleuritic chest pain that develops within days after an acute infection and may radiate to the neck, left shoulder, and arm. It is alleviated by sitting and leaning forward and worsens with supine positioning and during inspiration or coughing. In addition to muscular pain and fever.
Diagnosis
- Physical examination and heart auscultation
Pericardial friction rib is an intermittent, variable, scratchy cracking sound that is heard with the diaphragm of the stethoscope, more clearly on the left border of the sternum, during atrial and ventricle systoles and early ventricular diastole.
Stage 1: during the initial hours and days, wide ST elevation, along with ST depression on V1 and AVR, is detected. In addition to PR elevation on AVR and PR depression at V5 and V6, ECG changes may be normalized directly after this stage in self-limited cases.
Stage 2: During the first week, the ST segment and PR interval tend to normalize.
Stage 3: T wave inversion is noticed.
Stage 4: ECG changes may be normalized after appropriate treatment.
However, some patients may have a normal ECG, especially if acute pericarditis is not associated with inflammation of the epicardium.

- Echocardiography: may be used to detect any pericardial effusion, and to confirm any suspected cardiac tamponade or myocarditis.
- Cardiovascular magnetic resonance (CMR) and cardiac computed tomography (CCT) may be helpful in the evaluation of pericardium thickness.
- Laboratory workout:
- Elevated C-reactive protein, erythrocyte sedimentation rate, and leukocytosis may be noticed if infection is the underlying cause of acute pericarditis.
- Blood cultures may be collected and tested when sepsis is suspected.
- HIV and hepatitis C virus serology may be tested if suspected.
- Antinuclear antibody (ANA) titers may be tested when autoimmune disorders are suspected.
- Cardiac biomarker troponin may be acutely elevated in acute pericarditis cases.
References


.webp)
.webp)
.webp)
.webp)
.webp)

.webp)