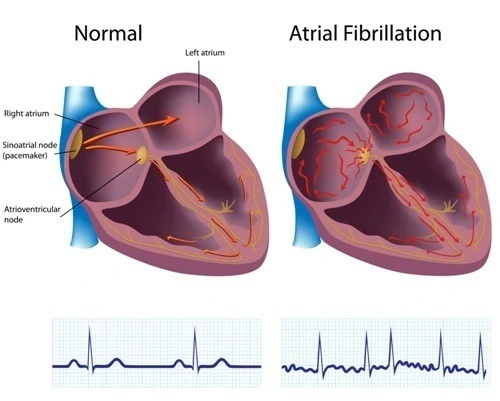
Heart arrhythmia is a cardiac condition where the beat rate or rhythm becomes abnormal and is caused by an irregularity in the origination of electrical signals or conduction. As a result, the patient may complain of many symptoms, and other cardiac and cerebral complications may develop. Also, it can be severe and life-threatening. Atrial fibrillation and Flutter are common arrhythmia types that originate from the atrium and cause tachycardia that is associated with elevated stroke risk.
Atrial Fibrillation
Since atrioventricular valvular disease, ventricular dysfunction, and ischemia may elevate arterial pressure, that will enhance atrial remodeling and result in atrial fibrillation.
ACC/AHA Classification
Classification of atrial fibrillation episodes that are not related to reversible or secondary causes:
- Paroxysmal Atrial Fibrillation: episodes that are terminated within less than 7 days, and usually, they terminate spontaneously.
- Persistent Atrial Fibrillation: recurrent episodes that are sustained longer than 7 days, and they may require pharmacological therapy or cardioversion.
- Long-lasting persistent atrial fibrillation: arrhythmia lasts longer than 12 months due to failure or inadequacy of cardioversion.
- Permanent Atrial Fibrillation: If atrial fibrillation resulted in permanent structural heart changes that led to the decision of treatment abortion.
Atrial fibrillation is associated with atrial remodeling, as electrical remodeling results in the shortening of the refractory period to allow a higher heart rate, besides reducing the velocity of atrial blood outflow. Also, multiple atrial contractibility changes weaken atrial contraction, blood stasis, and thromboembolism risk. In addition to structural remodeling through atrial dilation and increasing glycogen deposition, myolysis, and atrial dysfunction.
Anatomical reentry and spiral wave functional reentry mechanisms have a major role in atrial fibrillation pathogenesis when some cardiac fibers differ in their electrical properties, which affects the signal conduction pathway.
Atrial Flutter
- Typical type 1 Atrial Flutter
It occurs due to the formation of a counterclockwise or, in rare conditions, clockwise reentry circuit around the tricuspid valve annulus in the right atrium due to the prolonged refractory period of cavotricuspid isthmus (CTI) tissue compared to the surrounding tissues.
- Atypical Type 2 Atrial flutter
It can be formed in either the right or left atrium, where tissues have different electrical properties, leading to reentry circuit formation. Usually, these electrical differences emerge as a result of underlying ischemia, along with premature atrial contractions.
Since the atrial beat rate is markedly increased in atrial flutter, the atrial-to-ventricular beat ratio will be 2:1, 3:1, or more, depending on the fact that the atrioventricular node can only conduct 180 electrical signals per minute as a maximum rate due to its long refractory period.
Clinical Presentation
Secondary causes such as hyperthyroidism and stimulant use can trigger atrial fibrillation and flutter episodes. Patients with atrial fibrillation and flutter usually suffer from palpitations, decreased exercise tolerance, general weakness, and syncope. In severe cases, patients may present with angina, chest pain, hypotension, and decompensated heart failure. Atrial flutter is usually associated with a higher heart rate, which affects ventricular systolic function and leads to decreased cardiac output.
Assessment and Diagnosis Approach
If atrial fibrillation and flutter are suspected, electrocardiography (ECG) must be done to confirm the diagnosis and detect any cardiac comorbidities, such as pre-excitation, branch blocks, left ventricular hypertrophy, and myocardial infarction. Also, transthoracic echocardiography (TTE) must be done to evaluate atrium size, ventricle size and function, and cardiac valve properties. In addition, transesophageal echocardiography (TEE) may be performed to detect any atrial thrombus.
ECG changes associated with atrial fibrillation:
- Heart rate is elevated to 80–180 bpm
- Heart rhythm is irregularly irregular
- The p wave is absent
- QRS complex may be affected if it is accompanied by abnormal intraventricular conduction
ECG changes associated with atrial flutter:
- Heart rate is elevated to 240–400 bpm
- Heart rhythm is usually regular
- A F-wave or saw tooth pattern may be detected.
- In inferior leads (II, III, and aVF), positive flutter waves are observed in typical clockwise reentry, and negative flutter waves are observed in typical counterclockwise reentry
- In V1 lead, a negative flutter wave is observed in typical clockwise reentry, and a positive flutter wave is observed in typical counterclockwise reentry
- These waves are absent in atypical Atrial flutter
- Some degree of atrioventricular block may be detected
References


.webp)
.webp)


.webp)



.webp)

.webp)



.webp)