Premature atrial contractions are a condition also known as premature atrial complexes (PACs), premature atrial beats, premature supraventricular complexes, or premature supraventricular beats. It represents the activation of the atria from another site than the sinus node. It is triggered by the atrial myocardium and might happen to a wide variety of people.
Symptom Assessment
PAC is usually asymptomatic and can be discovered incidentally through routine checkups, except in some individuals, where it may cause skipping sensations and palpitations. These palpitations happen when there is a pause and increase in left ventricular inotropy that is a result of a stroke volume increase
Dizziness, lightheadedness, and presyncope might happen due to bradyarrhythmia, which is a result of atrial bigeminy and nonconducted PAC. Ventricular rates could reach 40 beats per minute.
When PAC coexists with bradycardia, it might produce a hemodynamic compromise.
Some patients experience anxiety, shortness of breath, and other signs and symptoms of heart failure.
Physical examination
Irregular pulses are the most common finding; premature pulse waves or pauses might be detected when the peripheral pulse is examined. There might also be some changes in the timing and intensity of several cardiac murmurs.
Early non-conducted PACs can be distinguished from sinus pauses by examining the venous jugular pulsation and the presence of cannon A wave is key evidence of early PACs.
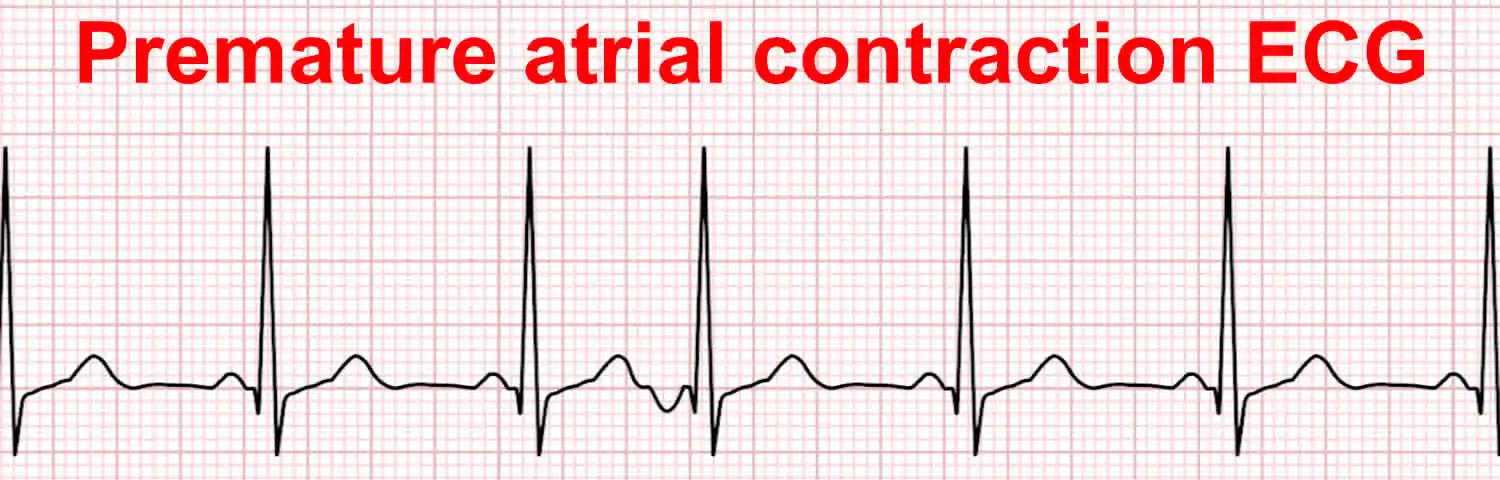
Electrocardiogram and Evaluation
It is considered the standard method for identifying electrical variations.
- PACs appear as a P wave that differs from the sinus P wave in its morphology and axis.
- Normal QRS interval and longer or shorter PR interval depending on the origin site. A shorter PR interval (< 120 ms) originates in the low right atrium near the AV node. Inspecting multiple or all leads might be essential to distinguishing differences.
- Fast baseline heart rates result in a hidden abnormal P wave, producing a "camel hump" or "peak" T wave that, if it isn't recognizable by the physician, will be mistaken for junctional premature beats (JPBs).
- Conducted a widened QRS complex. Right bundle branch block aberrancy is more frequent than left bundle branch block aberrancy.
- No QRS complex. (non-conducted PAC).
- PAC might arise from one or several locations (unifocal or multifocal).
- A negative P wave in the inferior leads is a suggestion of low atrial focus.
- A negative P wave in both lead I and aVL is a suggestion of left atrial origin.
- Laboratory testing should be done to detect electrolyte abnormalities.
- Patients with frequent PAC should be evaluated for structural heart disease for its importance in treatment and prognosis.
Diagnosis
A "P" wave occurs earlier than the anticipated sinus P wave. This P wave has a different morphology from the sinus P wave, but it might appear similar to the normal sinus P if the ectopic focus is near the sinus node.
References:
- https://www.uptodate.com/contents/supraventricular-premature-beats
- https://www.ncbi.nlm.nih.gov/books/NBK559204/


.webp)
.webp)


.webp)



.webp)

.webp)



.webp)