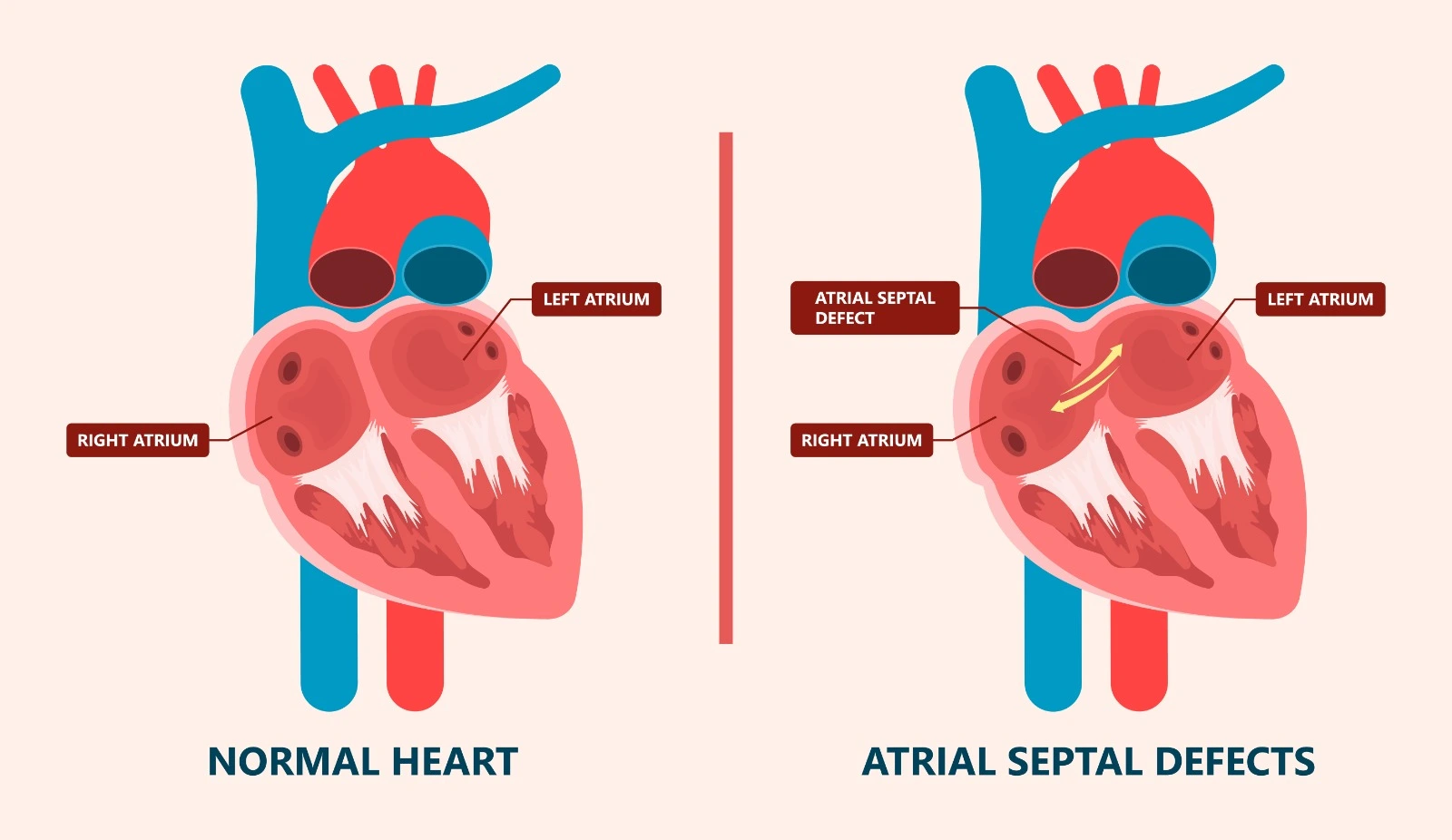
The septum is the wall that separates the two sides of the heart. During fetal life, there is a normal opening between the two atria where oxygenated blood from the maternal placenta can move directly from the right atrium to the left atrium and then to circulatory circulation, bypassing pulmonary circulation. This opening is normally closed completely within a few weeks or months after birth.
Occasionally, the opening in the septum between the right and left atria doesn’t close completely. It may have existed in healthy, normal people without any symptoms, as in Patent Foramen Ovale (PFO). Another congenital heart defect may result in a left to right shunt and leakage of oxygenated blood from the left to the right atrium during ventricular late systole and early diastole, which increase the pressure in the pulmonary circulation and cause pulmonary vessel damage, as in Atrial Septal Defect (ASD).

Atrial Septal Defect Types
Atrial septal defects are classified into many types, which include:
- Ostium secundum is considered the most common atrial septal defect type, where the adhesion of the flap valve is not complete in the middle of the wall between the two atria. It is associated with Patent Foramen Ovale.
- Ostium primum, where the opening is at the lower part of a wall between the two atria near the atrioventricular node, affects the septal cusp of the mitral valve. Also, it may be associated with other congenital heart defects.
- Sinus venous is considered a rare type of atrial septal defect, where the defect is in the upper part of the wall separating the heart atria, near the entry of the superior vena cava. It's also associated with other congenital heart structural changes.
- The coronary sinus is a rare type of atrial septal defect where a missing wall part is between the coronary sinus—a part of the heart venous system—and the left atrium, so the left superior vena cava will drain blood into the left atrium.
Etiology
An atrial septal defect is considered a congenital heart defect where the direct underlying cause is unknown, although some risk factors are associated with the condition, which include:
- A family history of congenital heart defects
- Rubella or German measles infection during the first months of pregnancy
- Systemic Lupus Erythematosus
- Diabetes Mellitus
- Tobacco and alcohol use
- The use of antiepileptic and mood stabilizer medications
Clinical presentation and complications
The degree of symptoms is dependent on the size of the septum opening, as a larger opening size will decrease the left atrium pressure to the same level as the right atrium pressure. Also, it may be associated with other heart defects. Patients with large atrial septal defects may present with dyspnea, exercise intolerance, perceived heartbeats, or feeling like some beats are not completed.
An atrial septal defect is associated with elevated pulmonary hypertension, a reverse shunt as in Eisenmenger syndrome, and an increased risk of bronchitis and pneumonia. Also, it may lead to peripheral or abdominal edema and heart failure. In advanced cases, patients may experience atrial arrhythmia and syncope episodes. Furthermore, some ischemic stroke and transient ischemic attack cases are linked with Patent Foramen Ovale. In addition, it may be associated with early death.
Diagnosis
- Heart sounds Auscultation may reveal:
- Split S1 heart sound due to delayed tricuspid valve closure.
- Split and fixed S2 heart sound due to delayed pulmonary valve closure.
- S4 heart sound may present due to right ventricular hypertrophy and pulmonary hypertension.
- Heart murmurs at the left of the sternum in the second intercostal space.
- Hyperdynamic impulse of right ventricular due to increased filling.
- A palpable impulse from a distended pulmonary artery may be detected upon physical examination.
- Chest radiography (CXR) may show cardiomegaly and a prominent pulmonary artery.
- Magnetic resonance imaging (MRI) can identify the size and position of significant atrial septal defects. Also, it can assess right ventricular size and function and systemic and pulmonary venous return.
- Transthoracic echocardiography (TTE) is used to confirm the diagnosis of most types of atrial septal defects.
- Transesophageal echocardiography (TEE) is used for the diagnosis of sinus venosus, a type of atrial septal defect.
References


.webp)
.webp)


.webp)



.webp)

.webp)



.webp)