Overview
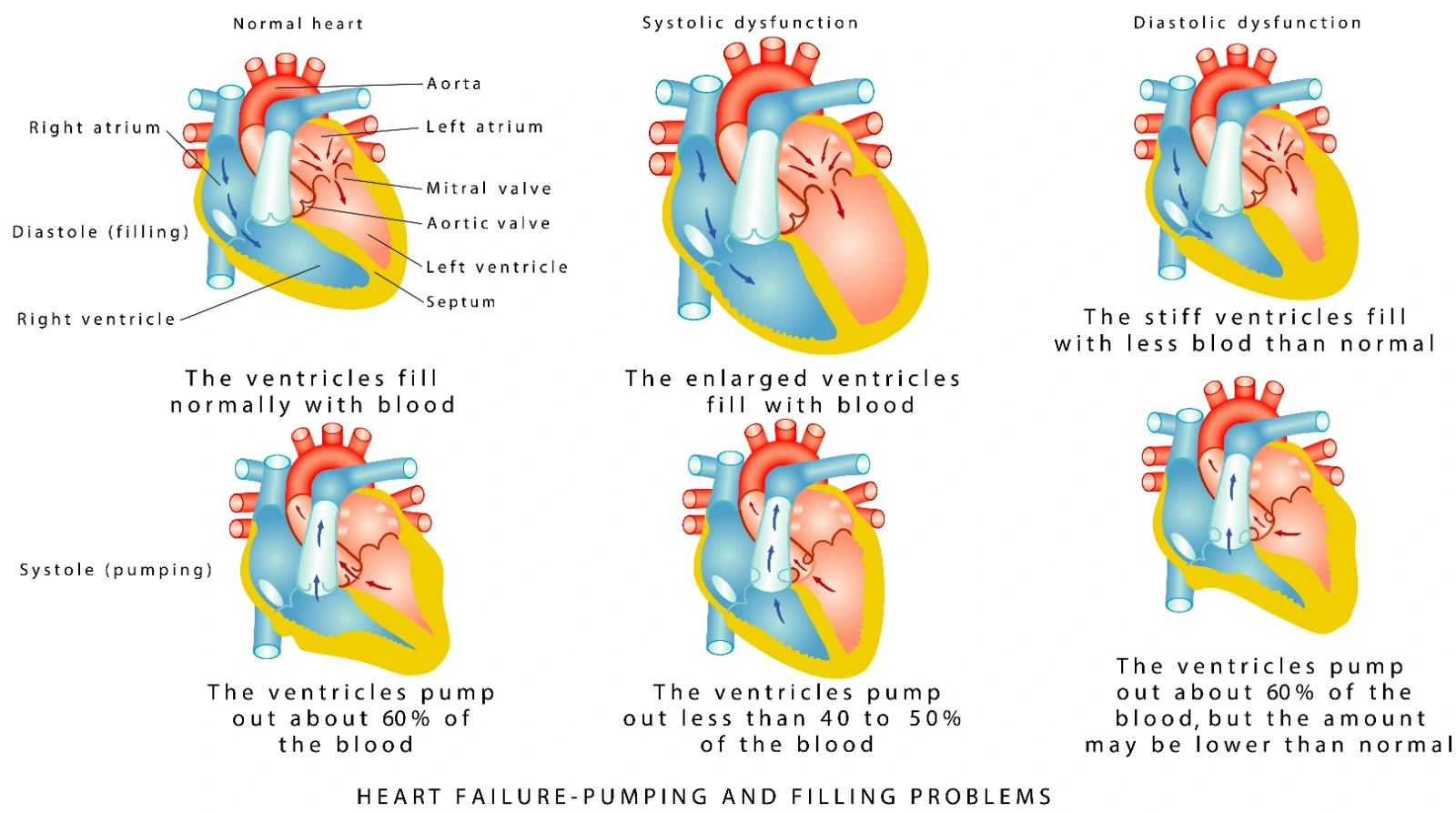
Systolic heart failure, also known as heart failure with reduced ejection fraction (HFrEF), is defined as heart failure with an ejection fraction of ≤ 40%. It happens due to a defect in the heart's ability to contract properly, resulting in decreased cardiac output.
Dilated cardiomyopathy is the dilation and impairment of the contraction of one of both ventricles of the heart, and it might be the leading cause of heart failure (overt heart failure).
HFrEF can be caused by ischemic heart disease (IHD), dilated cardiomyopathy, hypertension, or valvular heart disease. Whereas unexplained dilated cardiomyopathies (CMP) might have different etiologies: idiopathic CMP (most frequently), myocarditis, IHD, infiltrative disease, peripartum cardiomyopathy, hypertension, HIV infection, connective tissue disease, substance abuse, doxorubicin, and other causes.
Stages of Heart Failure
- Stage A: At risk of Heart failure
- Stage B: Pre-Heart failure
- Stage C: Symptomatic Heart failure
- Stage D: advanced heart failure
As both stages A and B are asymptomatic, they are not considered a definitive diagnosis, as the patient should have current or prior symptoms to be diagnosed with heart failure.
Patients whose symptoms resolve are still considered Stage C heart failure patients.
Pathophysiology
The pathophysiology of HFrEF is mainly multiple compensatory responses that provide short-term support to maintain homeostasis of the body after acute development of blood pressure (BP) reduction and reduced renal perfusion. The compensatory mechanisms are:
- Tachycardia and increased contractility: Due to norepinephrine release in response to a drop In cardiac output, it also increases myocardial oxygen demand.
- Fluid retention and increased preload: activation of the RAAS system due to low renal perfusion; this leads to activation of angiotensin II and vasoconstriction, leading to salt and water retention and increased ventricular volume and pressure.
- Vasoconstriction and increased afterload: NE, angiotensin II, endothelin-1, and arginine vasopressin are responsible for the vasoconstriction that prevents blood from being ejected from the ventricle, which leads to worsening of cardiac output and an increase in the afterload that eventually leads to more worsening of HF.
- Ventricular hypertrophy and remodeling: changes in size, shape, and structure of the heart that diminish the performance of the heart.
Dilated Cardiomyopathy Systolic dysfunction happens because of the inability of the heart to maintain a normal cardiac output, which eventually leads to dilatation of the ventricle. The excessive pressure eventually leads to reduced contractions and remodeling. Remodeling might happen due to certain genotypes or cardiac injury.
Clinical Manifestations of Heart Failure
Dyspnea, ascites, orthopnea, hepatic congestion and pain, fluid retention, and pulmonary edema (crackles).
Diagnosis of HFrEF
- History and physical examination: vitals, volume assessment, and cardiac examination
- Echocardiogram: it can identify causes of HF, and atrial and ventricular sizes are helpful.
- BNP: patients with heart failure and dyspnea usually have values above 400 pg/mL.
- NT-proBNP: usually fourfold BNP.
- Hemodynamic exercise test: usually not required unless the diagnosis is uncertain despite initial evaluation. In this case, heart failure symptoms and PCWP >= 15 mmHg at rest or >= 25 mmHg during exercise are enough for diagnosis.
Diagnosis of Dilated cardiomyopathy
- Dilatation and impaired systolic function
- Myocyte hypertrophy and replacement fibrosis with variable involvement of the conduction system.
- Genetic testing and family screening.

Management of HFrEF
Patients with NYHA II-III (add medications sequentially, not all at once):
- ARNI : Sacubitril-Valsartan, THEN ADD
- Beta-blocker, THEN ADD
- Mineralocorticoid receptor antagonist, THEN ADD
- Sodium-glucose co-transporter 2 inhibitor
Management of Dilated Cardiomyopathy
- Secondary prevention of sudden death:
For patients with dilated CMP who survived a cardiac arrest or ventricular arrhythmia causing hemodynamic instability: an implantable cardioverter defibrillator is recommended.
- Primary prevention of sudden death:
- DCM, heart failure, and LVEF <=35% with at least 3 months of optimal medical therapy: an implantable cardioverter defibrillator should be considered.
- DCM and genotype with high sudden cardiac death risk, LVEF >= 35%, and additional risk factors (table below): Implantable cardioverter defibrillator should be considered.
- DCM and genotype with high sudden cardiac death risk, LVEF >= 35%, and no additional risk factors: an implantable cardioverter defibrillator may be considered.
- DCM with no genotype, high sudden cardiac death risk, LVEF >= 35%, and no additional risk factors: an implantable cardioverter defibrillator may be considered.
References:
- https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Focused-Update-on-Heart-Failure-Guidelines
- https://www.uptodate.com/contents/causes-of-dilated-cardiomyopathy
- Pharmacotherapy: A Pathophysiological Approach, 12th edition
- https://www.uptodate.com/contents/determining-the-etiology-and-severity-of-heart-failure-or-cardiomyopathy
- https://www.jacc.org/doi/pdf/10.1016/j.jacc.2021.12.012?_ga=2.223030491.1129219989.1697546937-100308460.1697546937
- https://www.uptodate.com/contents/heart-failure-clinical-manifestations-and-diagnosis-in-adults
- https://www.uptodate.com/contents/familial-dilated-cardiomyopathy-prevalence-diagnosis-and-treatment
- https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Cardiomyopathy-Guidelines
- https://www.uptodate.com/contents/primary-pharmacologic-therapy-for-heart-failure-with-reduced-ejection-fraction
- https://www.ncbi.nlm.nih.gov/books/NBK553848/


.webp)
.webp)


.webp)



.webp)

.webp)



.webp)